Thu, Feb 12, 2026
Volume 11 - Continuous Publishing
Iran J Neurosurg 2025, 11 - Continuous Publishing: 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghiasi Y, Liew Y Y, Abdollahzade S, ray A. CT Scan-based Morphometric Study of Cervical Screw Placement in the Iranian Population. Iran J Neurosurg 2025; 11 : 13
URL: http://irjns.org/article-1-459-en.html
URL: http://irjns.org/article-1-459-en.html
1- Student Research Committee, Qazvin University of Medical Sciences, Qazvin, Iran.
2- Department of Neurosurgery, Royal Preston Hospital, Lancashire Teaching Hospitals NHS Foundation Trust, Preston, United Kingdom.
3- Department of Neurosurgery, Royal Preston Hospital, Lancashire Teaching Hospitals NHS Foundation Trust, Preston, United Kingdom. & Department of Surgery, School of Medicine, Qazvin University of Medical Sciences, Qazvin, Iran ,sina21@gmail.com
2- Department of Neurosurgery, Royal Preston Hospital, Lancashire Teaching Hospitals NHS Foundation Trust, Preston, United Kingdom.
3- Department of Neurosurgery, Royal Preston Hospital, Lancashire Teaching Hospitals NHS Foundation Trust, Preston, United Kingdom. & Department of Surgery, School of Medicine, Qazvin University of Medical Sciences, Qazvin, Iran ,
Keywords: Cervical spine, Computed tomography (CT) morphometry, Transpedicular screws, Translaminar screws, Lateral mass screws
Full Text [PDF 1866 kb]
(337 Downloads)
| Abstract (HTML) (1384 Views)
Full Text: (121 Views)
Introduction
The stability of the cervical spine can be affected by multitudes of pathologies, including, but not limited to, trauma, malformations, tumors, and osteoarthritis. An unstable cervical spine might mandate surgical intervention in the form of stabilization and fusion. To stabilize the cervical spine, surgeons have used different methods and devices through the posterior approach. These procedures are commonly undertaken for pathologies affecting sub-axial cervical vertebrae [1-5].
Most spinal surgeons use lateral mass screws (LMS) for sub-axial cervical vertebrae stabilization, as it provides excellent stability whilst maintaining a high fusion rate [6-8]. LMS has been associated with loosening or erosion, which may require further fixation of the screws into the pedicle [9, 10]. Laminar screws are also increasingly used in the treatment of cervical pathologies [11].
The most reliable technique for stabilizing the spine is transpedicular screw fixation (TPSF) [12, 13]. However, it presents a unique challenge in the cervical region due to the proximity of the pedicles to eloquent structures, such as vertebral arteries, spinal cord, and nerve roots. The complexity of cervical spine anatomy is due to pedicle dimension and angulation variations among various ethnicities and proximity to vital neurovascular structures [14, 15]. A thorough understanding of the morphometric features of the cervical spine is essential for any spine surgeon dealing with it and crucial for implant design and development [16-18]. Pedicle screws provide higher biomechanical stability, while LMS are more straightforward to place [19, 20]. These, along with laminar screws, are key parts of any spine surgeon’s toolkit to deal with this complex region of the spinal column through a posterior approach.
A good understanding of the cervical anatomy is required for successful insertion of any type of screw to avoid damage to nearby elements, such as spinal cord injury, durotomy, vascular injury, and inadequate bone purchase that may predispose the implant to loosening, pull out, and eventual failure [14, 21]. Before any surgical interventions, surgeons will evaluate the anatomy of the vertebrae using a computed tomography (CT) scan to determine the size, shape, and angle of the pedicle. This is increasingly important for the management of deformity cases where the characteristics of a normal spinal anatomy are probably deranged [22].
Studies have shown that there are significant differences in terms of morphometric measurements between races and genders, emphasizing the importance of studying the morphometry of the vertebrae in different populations to increase the safety and accuracy of surgery [23]. Despite existing data from other ethnic groups, there is limited information on the morphometry of the cervical spine in the Iranian population. These anatomical variations are critical for safe screw placement in spinal surgery. This is especially important in Iran, where spinal screws are mostly not locally manufactured and are imported, often based on foreign anatomical standards. Therefore, this study evaluates the feasibility of transpedicular, translaminar, and lateral mass screw placement by assessing morphometric characteristics in a representative Iranian sample using CT imaging, to evaluate the differences between the existing screws and actual population cervical spinal morphometry.
Methods and Materials/Patients
Study design
This was a cross-sectional, retrospective morphometric study conducted on CT images obtained from Rajaei Hospital, Qazvin, Iran, PACS records.
The simple random sampling was used to select 100 CT scans from adult patients who met the inclusion criteria. Cervical CT scan imaging of 100 adult patients (above 18 on enrolment day) who underwent CT imaging for various clinical reasons (e.g. trauma) and were referred to Rajaei Hospital in Qazvin City, Iran, was retrospectively reviewed in this cross-sectional study. The exclusion criteria were as follows: 1) Non-standard and low-quality CT scan; 2) Vertebral fracture; 3) Pre-existing pathologies of the cervical spine, including infection, rheumatoid arthritis, or masses in the vertebrae; 4) History of surgery on the spine; and 5) Ankylosing spondylitis.
Measurements including the length, width, height, and placement angles of the three types of screws (transpedicular, translaminar, and lateral mass) of the subaxial cervical vertebrae were obtained from the cervical CT imaging.
Data collection
A checklist including age, sex, and measured parameters of the vertebrae was completed by the study manager, and the measurements were performed on the CT scan images using the Marco PACS division program (last version: 14.29.55).
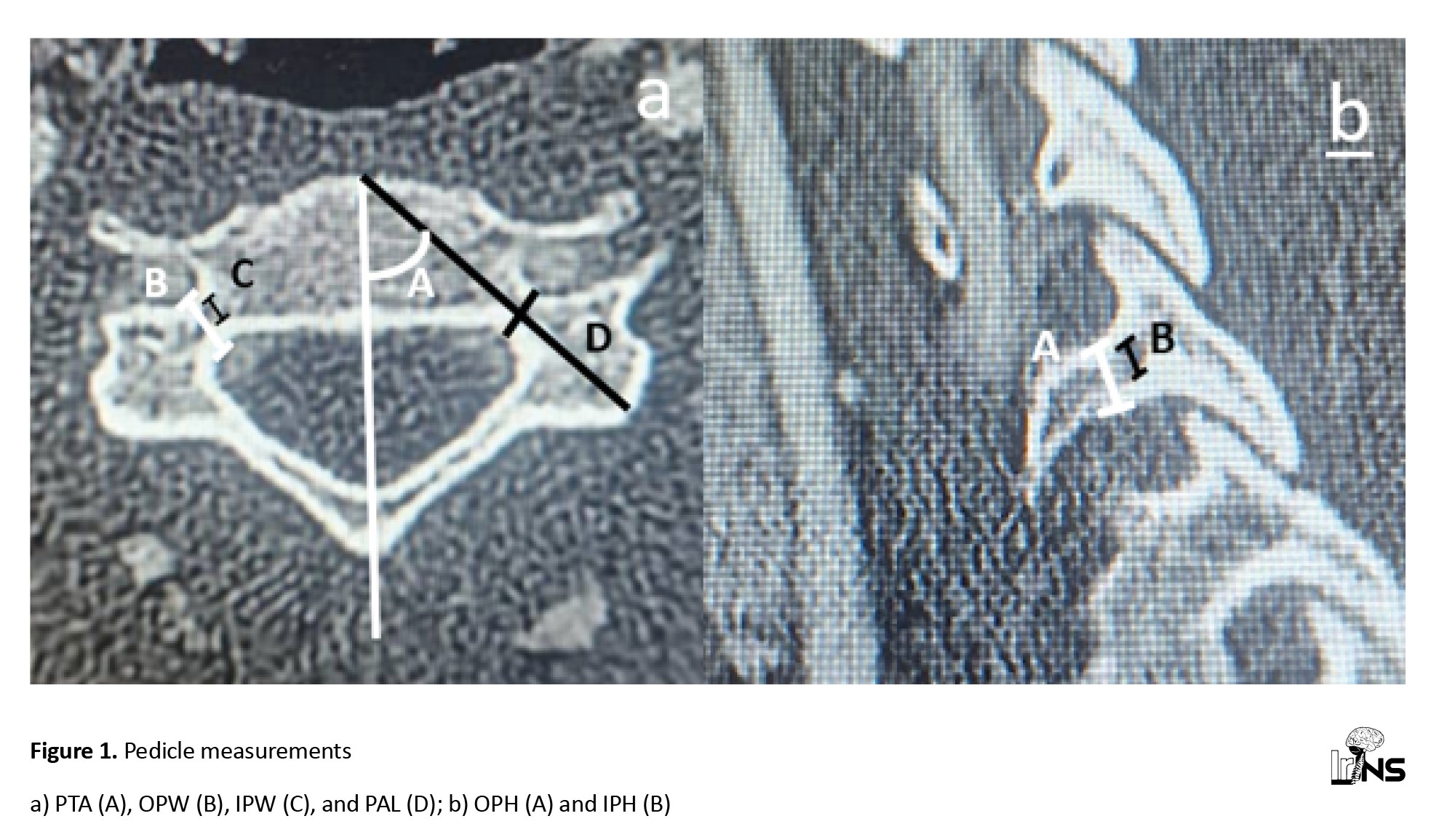
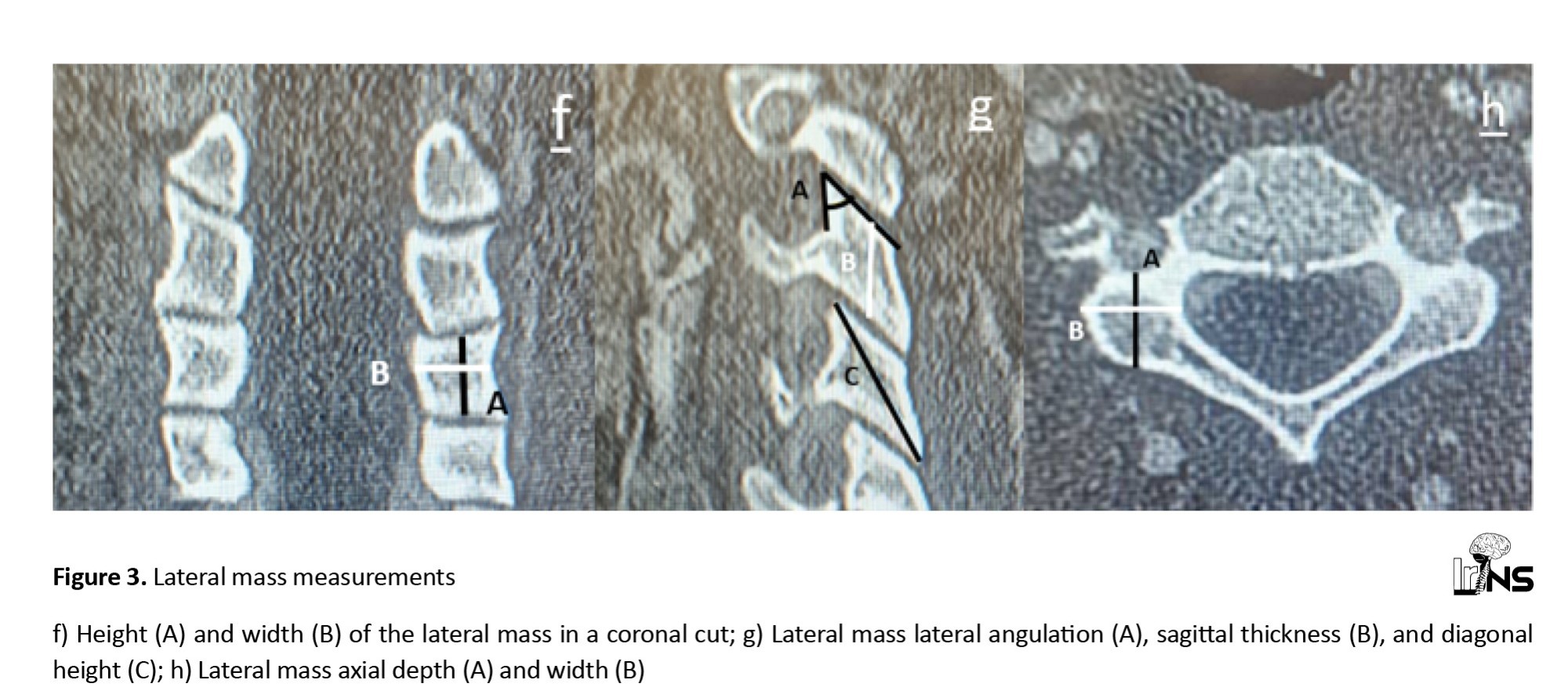
The parameters were measured on CT scan slices where their values were at their maximum, and the values were expressed in millimeters. The measured parameters are shown in the following figures (Figures 1, 2, and 3).
Statistical analysis
The collected data were entered into the computer using the SPSS software, version 19 (developed by IBM, version: 28.0.1). For descriptive results, the frequency, Mean±SD were calculated based on the type of the variables. The results were analyzed using an independent t-test and a chi-square test to examine the relationship between quantitative and qualitative variables. Meanwhile, a P<0.05 was considered significant.
Results
Baseline characteristics
In this study, the length, width, height, and placement angles of the three types of screws (translaminar, transpedicular, and lateral mass) of the subaxial cervical vertebrae of 100 patients were examined. A total of 58 patients (58%) were male and 42 patients (42%) were female. The mean age of the patients was 37.4±12.7 years and ranged from 18 to 67 years. Before examining the objectives, the distribution of data was checked in terms of normality using the Kolmogorov–Smirnov test, and the normal results were confirmed. The results of the study objectives were obtained in the following tables.
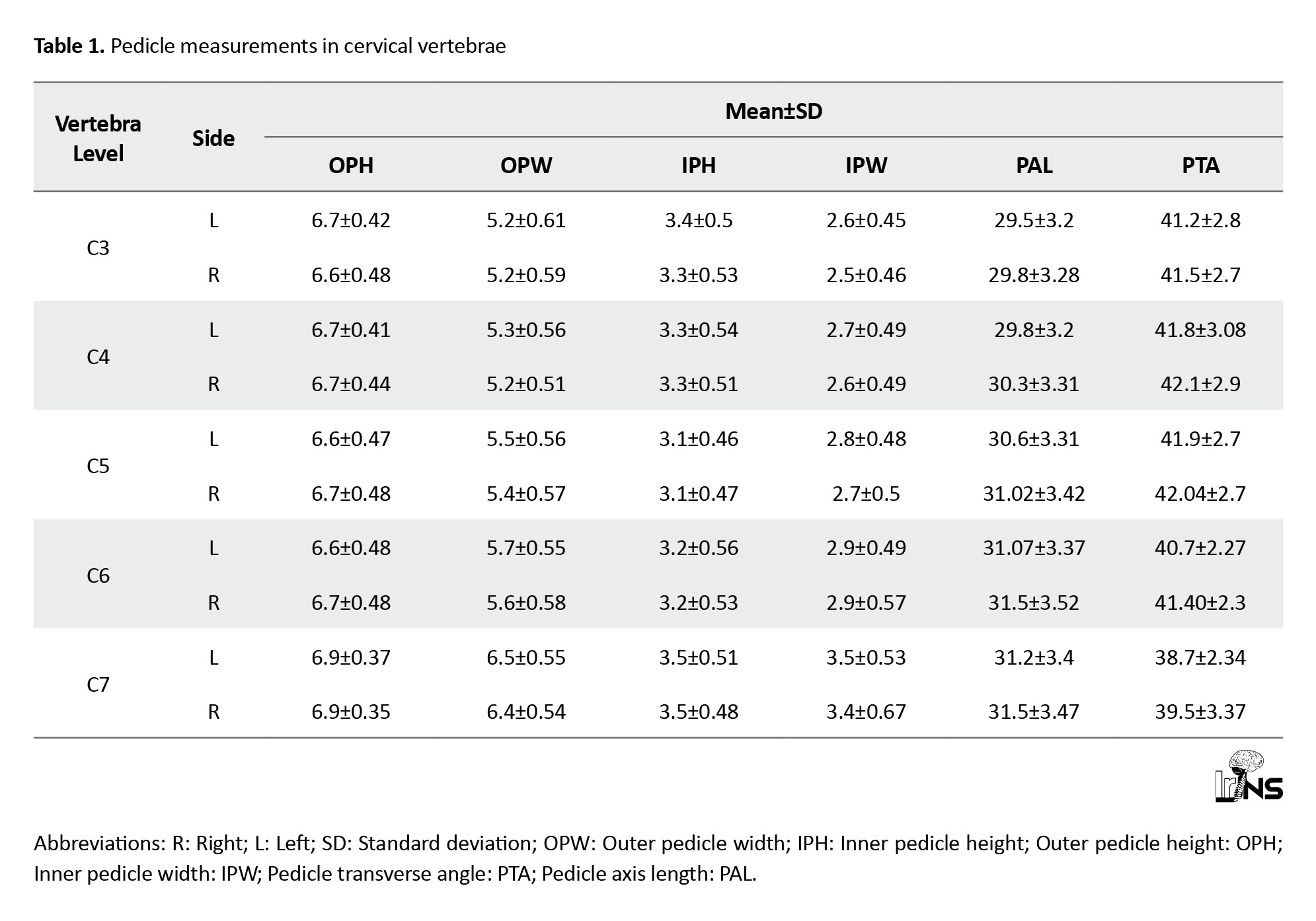
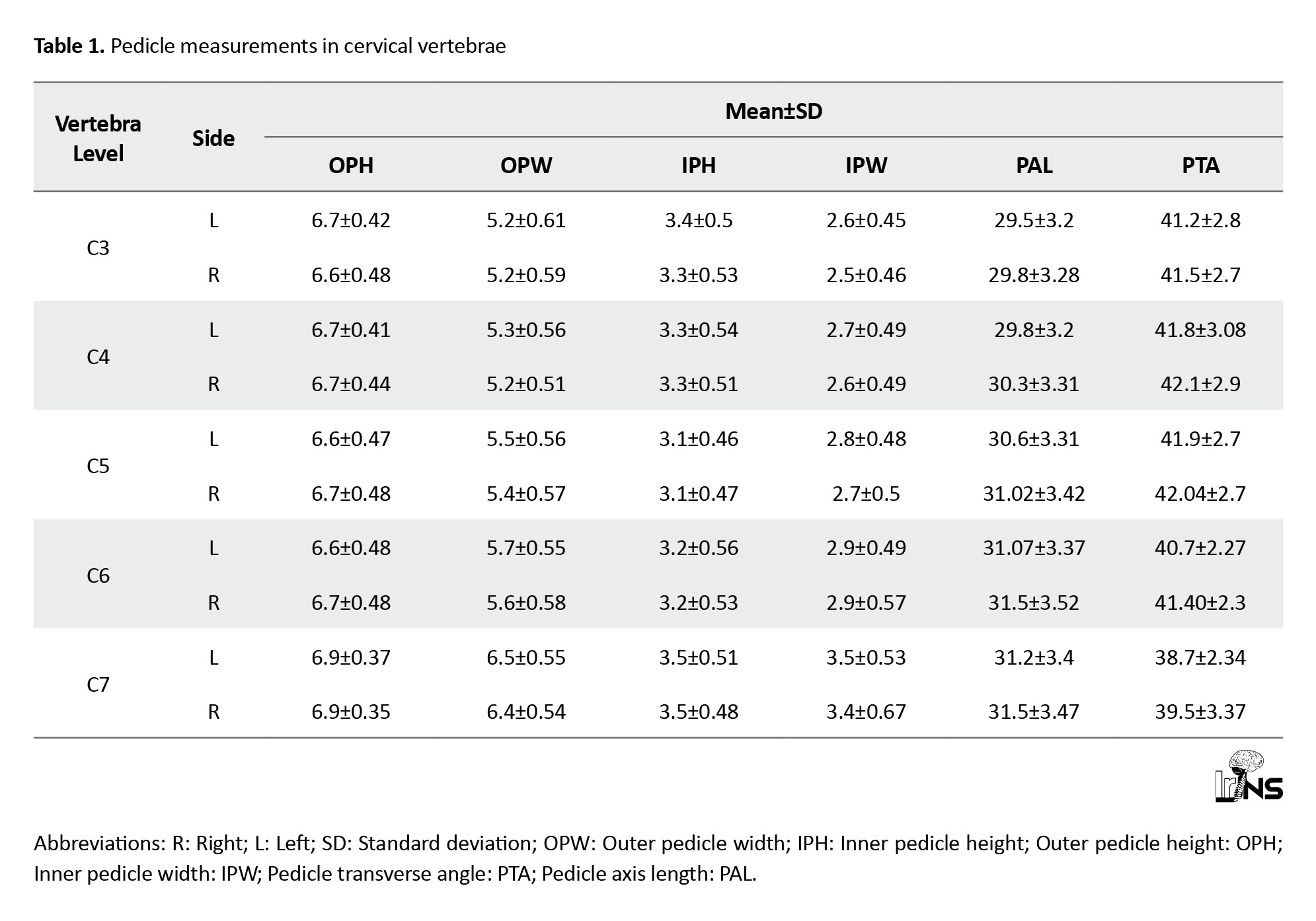
Mean outer pedicle height (OPH) on CT scan: The mean outer height of the pedicle isthmus was greatest at C7 and applied to both left and right. Mean outer pedicle width (OPW) in CT scan: The mean outer width of the pedicle isthmus was greatest at C7 and applied to both left and right.
Mean inner pedicle height (IPH) on CT scan: The mean inner height of the pedicle isthmus was greatest at C7 and applied to both left and right.
Mean inner pedicle width (IPW) on CT scan: The mean inner width of the pedicle isthmus was greatest at C7 and applied to both left and right.
Mean pedicle axis length (PAL) on CT scan: The mean distance from the posterior point of the pedicle axis on the lateral mass to the anterior margin of the vertebral body was greatest at C7 and was almost greater on the right side than on the left.
Mean pedicle transverse angle (PTA) on CT scan: The mean angle between the pedicle axis and the anatomical sagittal plane was greatest at C4 and C5 on the right side (Table 1).
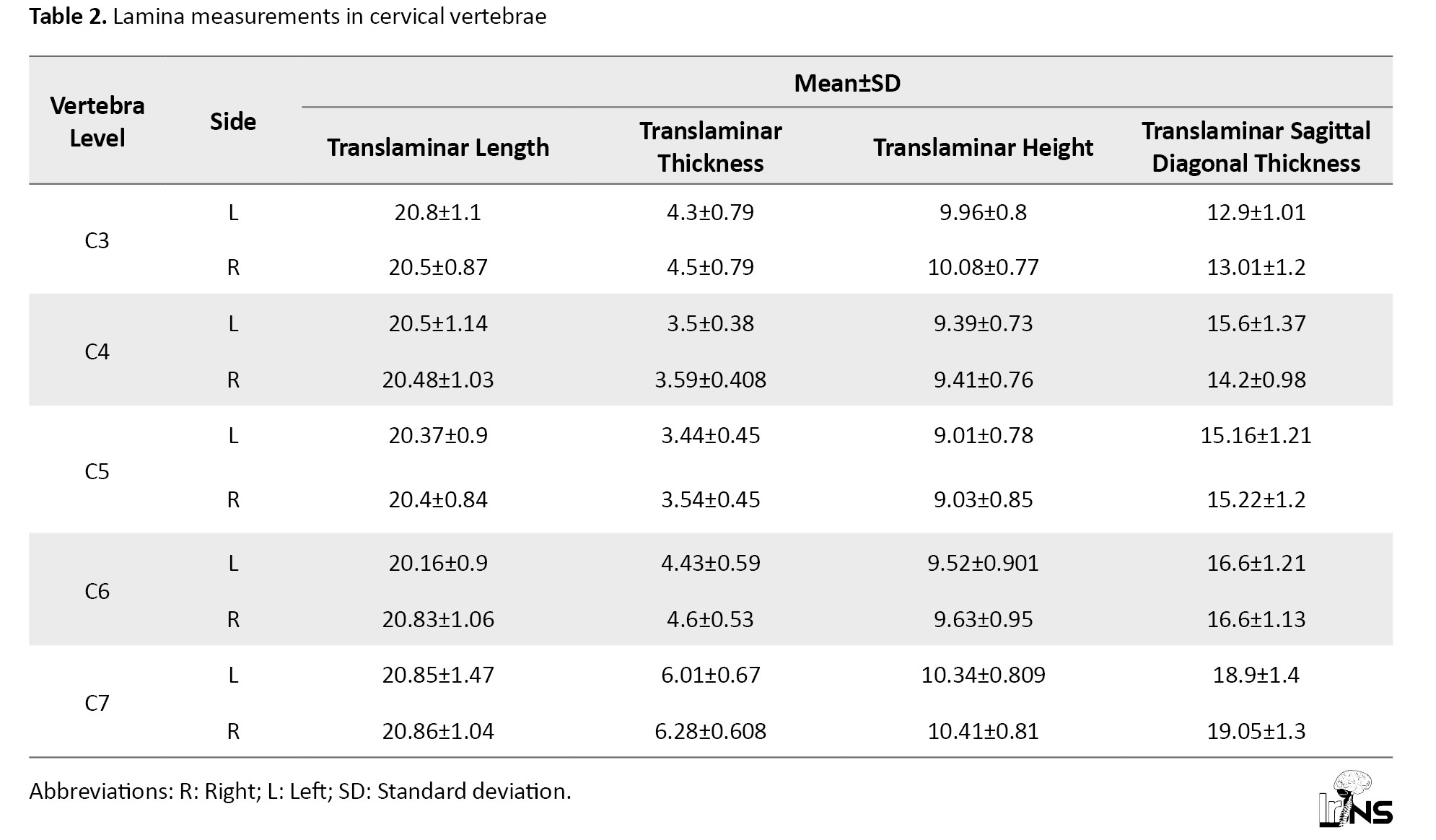
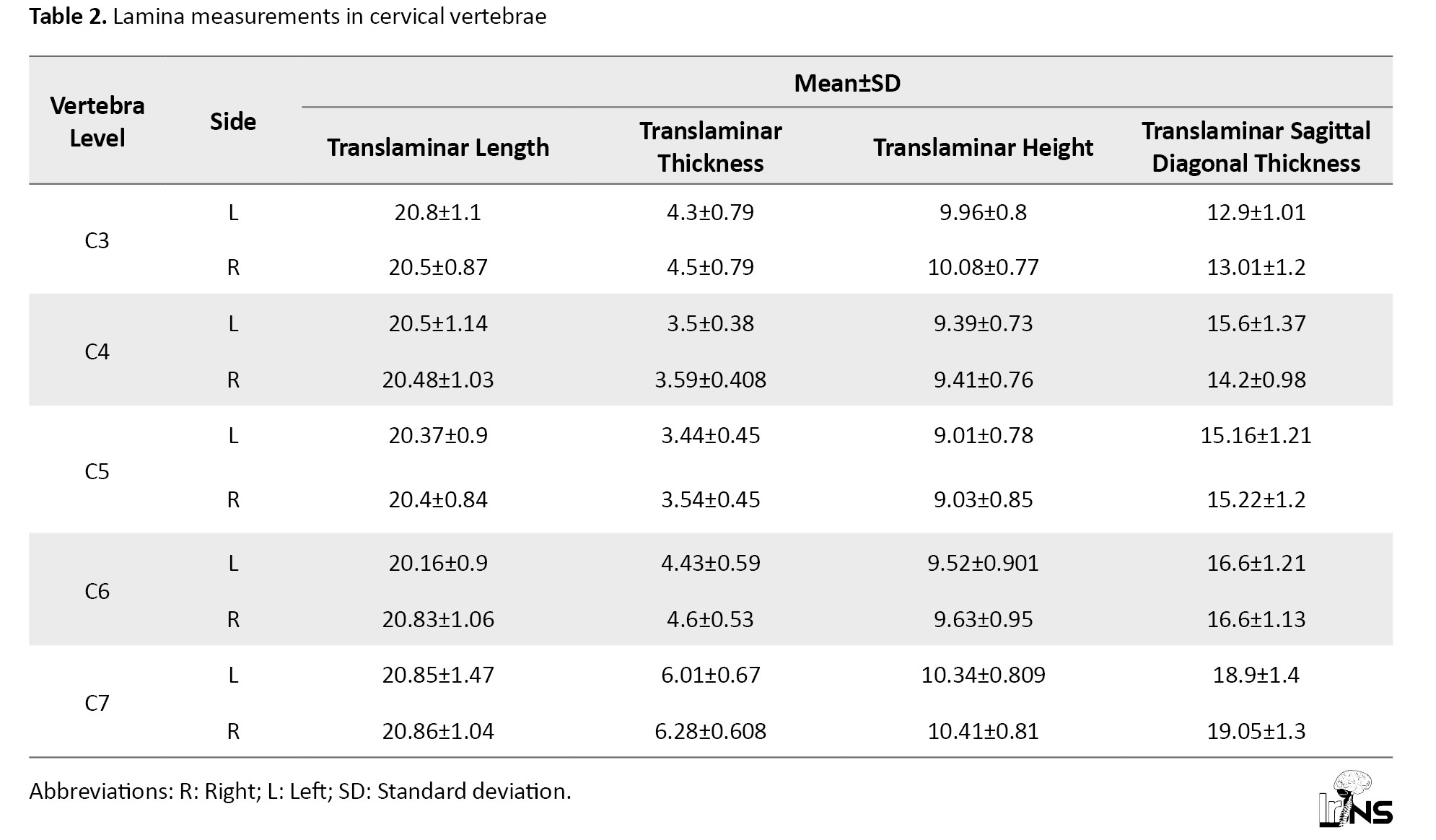
Mean translaminar length on CT scan: The mean translaminar length from the junction of the lateral mass and the lamina to the outer layer opposite the spinous process was greatest at C7 and was similar on the right and left sides. The average was higher at C3 on the left and C6 on the right.
Mean translaminar thickness on CT scan: The mean thickness or maximum distance from ventromedial to dorsolateral portions of the centre of the lamina was greatest at C7 and greater on the right side.
Mean translaminar height on CT scan: The mean maximum height between the spinous process and the base of the pedicle was greatest at C7 and was almost identical on the right and left sides.
Mean translaminar sagittal diagonal thickness on CT scan: The mean sagittal oblique distance from the most head point of the lamina to the tail end of it was greatest at C7 and was almost greater on the right side (Table 2).
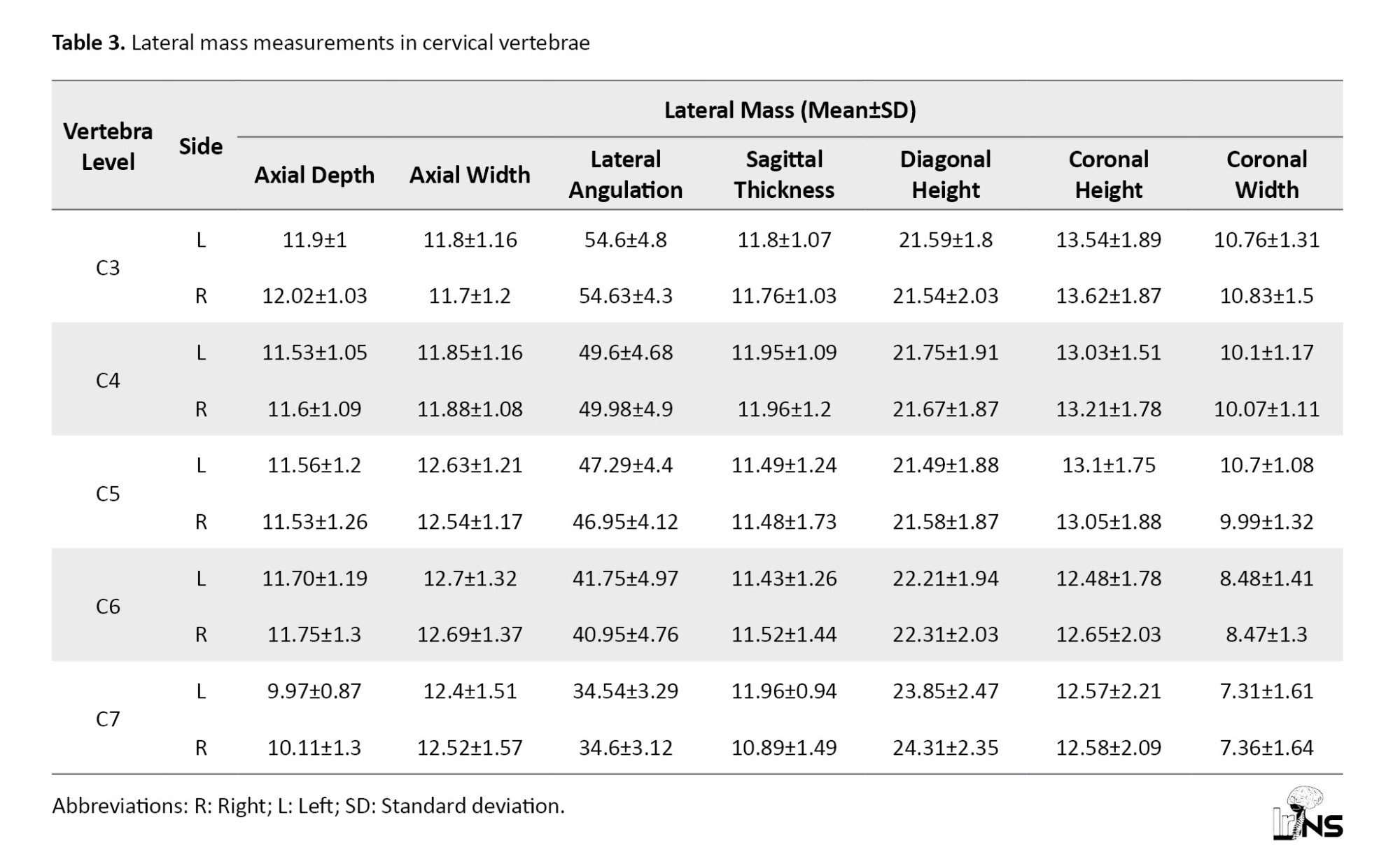
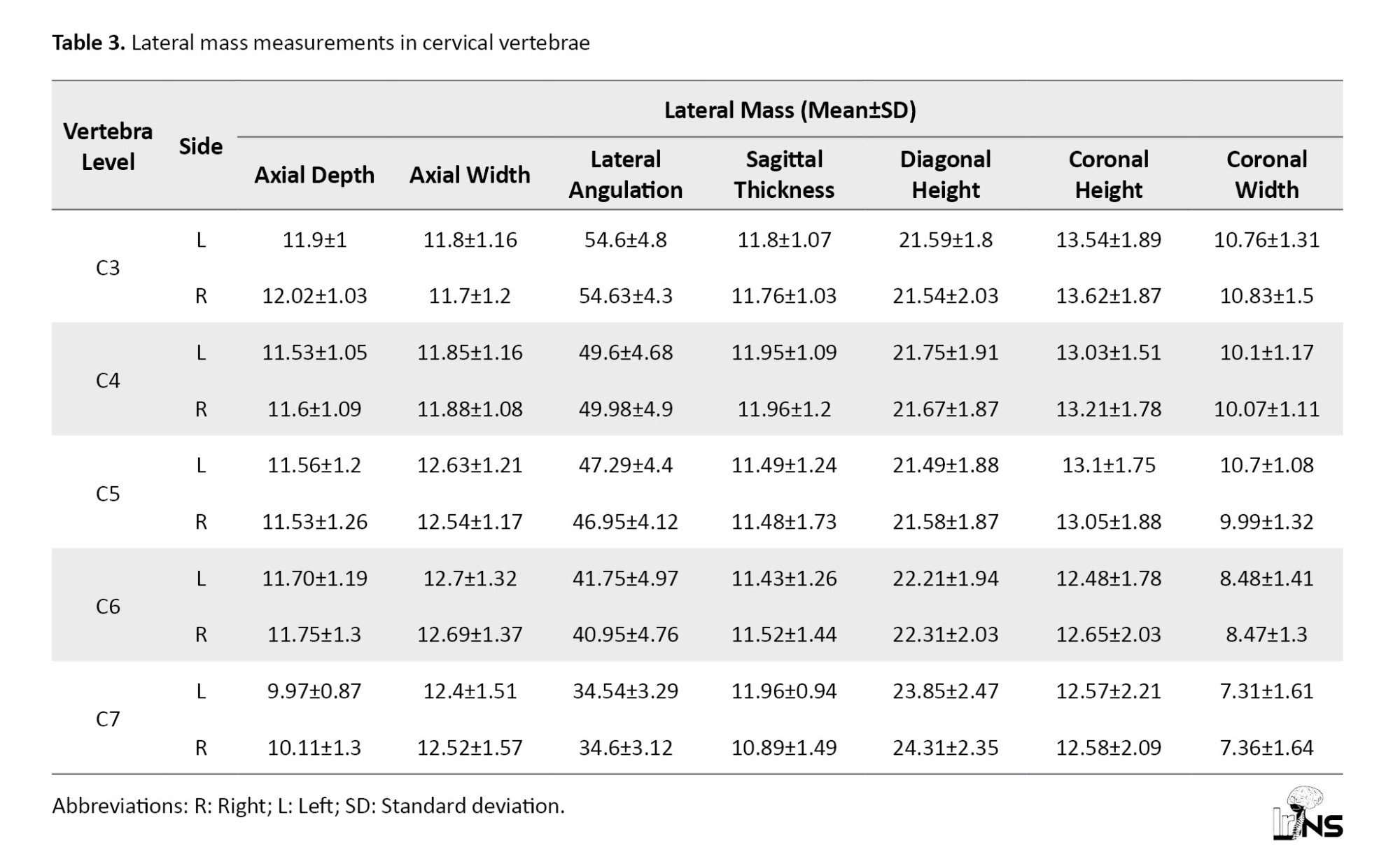
Mean lateral mass axial depth on CT scan: The mean anterior-posterior distance in the sagittal cut was greatest at C3 and almost greater on the right side.
Mean lateral mass axial width on CT scan: The mean internal-external distance in the sagittal cut was greatest at C6 and almost greater on the left side.
Mean lateral mass lateral angulation on CT scan: The mean medial distance above the centre of the lateral mass was greatest in C3 and was similar on the right and left sides.
Mean lateral mass sagittal thickness on CT scan: The mean thickness from the dorsal area to the ventral from the centre of the lateral mass was greatest at C7 and was almost greater on the left side.
Mean lateral mass diagonal height on CT scan: The mean distance from the tip of the superior articular facet to the inferior articular facet was greatest at C7 and greater on the right side.
Mean lateral mass coronal height on CT scan: The mean height of the head-to-tail distance from the centre of the lateral mass was greatest at C3 in the coronal cut and was greater on the right side.
Mean lateral mass coronal width on CT scan: The mean width of the internal-external distance in the coronal cut was greatest in C7 and was greater on the left side (Table 3).
Discussion
Overview of morphometric findings
Cervical fixation has been increasingly used in posterior approaches of the subaxial cervical region for multiple pathologies, and various techniques are utilized for this purpose, including lateral mass, pedicular, and translaminar screws. As the morphology of this complex region can be inconsistent among different ethnic groups, in the present study, the feasibility of inserting transpedicular, translaminar, and LMS was evaluated in the Iranian population.
This study demonstrates that the OPH, OPW, IPH, and IPW were measured to be highest at C7. The mean values of IPH and IPW were noted to be 3.5 mm and 3.4 mm, respectively, at C7. Whilst the mean IPH and IPW parameters were 3.5 mm at C7. Based on the findings of a review study by Liu et al., the mean OPW of the sub-axial spine in Asians was between 5.26-6.63 mm, and was between 5.17-6.64 mm in Europe/America [24].
Comparison with other populations
In a study by Al-Saeed et al., this morphometric parameter (OPW) had a mean of 5.8 mm at C7 in the Arab population [18]. These studies are consistent with the findings of the present study. In a 2014 study by Wasinpongwanich et al., OPH and OPW parameters were suitable for all sub-axial cervical spines with 3.5 mm screw placement [25].
In a recent study by Farooque et al. In 2018, CT scan results of 500 sub-axial cervical spines per 100 patients showed that the mean PW had the lowest value at C3 (4.3 mm) and highest at C7 (5.7 mm), which is coherent with the results of the present study. The study also showed that the mean PH had the lowest value at C3 (5.5 mm) and the highest at C7 (6.1 mm) [26], whilst in our study, C5 had the lowest mean IPW (OPW had the same mean value at C3, C5, and C6), and C7 had the highest mean IPW and OPW.
In a recent study by Alsaleh et al. In 2021, CT scan results in 207 patients suggested that the mean PW ranged from 4.4 mm at C3 to 6.1 mm at C7, and the mean PH ranged from 6.4 mm at C3 to 6.8 mm at C7 [27]. In the present analysis, mean OPW ranged from 5.2 mm at C3 to 6.5 mm at C7, and the mean OPH ranged from 6.6 mm at C3 to 6.9 mm at C7.
According to the present results, the PAL parameter had the highest value with a mean of 31.3 mm at C7. These findings are supported by Farooque et al. (2018), which showed that the mean PAL parameter was lowest at C3 (29.6 mm) and highest at C7 (33.04 mm) [26].
Measurements revealed that the PTA parameter, with an average of 42.1˚ had the highest value at C5. These parameters were similar on the left and right sides. This is in keeping with the findings from Chazono et al., which reported that the PTA was measured to be 37.1-49 degrees in the sub-axial spine in the Asian population and 38.7-48.8 degrees in the European/American population [9]. In the 2014 study by Wasinpongwanich et al., the results indicated that the PTA parameter had the highest value at C5 and the lowest value at C7, and the measurements were similar on both the left and right side [25]. In the study by Farooque et al. (2018), the mean PTA parameter was highest at C3 (44.58°) and lowest at C7 (37.18°) [26]. The data were comparable to the findings by Alsaleh et al. in 2021 [27]. Their study was able to show a varying mean PTA parameter of 42 to 51 degrees between different levels of C1-C7.
Although the pedicle width and height measurements of the Iranian population in our study were largely comparable to those reported in Arab, East Asian, and Western populations, subtle but clinically relevant differences were observed. For example, the mean OPW at C7 in our study was approximately 6.5 mm, compared to 5.8 mm in Arab populations and up to 6.6 mm in East Asian studies. This 0.5–0.7 mm variation may appear minor, but considering that cervical pedicle screws typically measure 3.5 mm in diameter, such differences can significantly influence the decision to proceed with pedicle screw placement. A narrower pedicle increases the risk of cortical wall violation, which potentially leads to neurovascular complications. These findings indicate the importance of obtaining population-specific morphometric data to guide preoperative planning, particularly in regions where generic or Western anatomical data are often used by default.
Translaminar morphometry
This study suggested that the thickness, height, and sagittal diagonal of the translaminar parameter were measured to have an average of 6.14, 10.37, and 18.97 mm at C7, respectively. On the other hand, the translaminar length parameter was averaged to be 20.65 mm at C3 and had the highest value at C7 (20.85 mm). Comparatively, in a study in 2015 by Ji et al., thickness, height, and diagonal- sagittal measurements of translaminar screw placement and feasibility analysis using one-sided and two-sided placement of 3.5 mm cervical screws on CT scan was assessed in 0.5 mm distance from the safety margin and the results showed that the translaminar length parameter with a maximum mean of 21.8 mm, the thickness parameter with an average of 6.1 mm, the height parameter with an average of 10.8 mm and the sagittal diagonal parameter with an average of 19.8 mm at C7 had the highest value [28]. The findings of the present study are in line with the study of Ji et al.
Lateral mass morphometry
Analysis of the data revealed that the depth and height of the lateral mass were highest at C3 with average values of 11.96 and 13.58 mm, respectively, and the axial width was noted to have an average of 12.69 mm at C6. In 2018, Patil et al. carried out a study on 104 patients in India to measure the lateral sub-axial cervical spine using axial, sagittal, and coronal CT scans, as well as anteroposterior and lateral x-rays. The results showed that the lateral masses were thinner and longer descending from C3 to C7 [29].
The results of the current study showed that the lateral mass parameters in lateral angulation and coronal height had the highest values at C3, with an average of 54.61 and 13.58 mm, respectively. In the study by Patil et al., they depicted that the lateral angulation was highest at C6 (24.4°) and lowest at C3 (22.7°). The coronal height parameter was measured to be the highest at C3, with an average of 12.9 mm [29].
According to the other findings of this study, the lateral mass sagittal thickness had the highest average value at C4 (11.95 mm), whilst the coronal width had the highest value at C3, averaging 10.79 mm and the lateral mass diagonal height had the highest value at C7 (24.08 mm). In the study by Patil et al., the sagittal incision thickness and the oblique length increased from C3 to C7. In their study, the sagittal incision thickness of 18 mm, and diagonal height parameter of 22.8 mm, and the coronal width parameter of 12.4 mm in C7 had the highest value [29].
Clinical implications
Based on the morphometric data, pedicle screw placement appears most feasible at the C7 level due to wider pedicle dimensions (OPW/IPW ~6.5/3.5 mm), which allows the surgeon to safely insert 3.5 mm screws with acceptable margins. At higher levels, such as C3–C5, where pedicle dimensions are narrower, lateral mass or translaminar screws are likely safer and preferable. The observed PTA values (up to ~42° at C5) provide intraoperative guidance for angulation to avoid cortical breaches. These data can help neurosurgeons in preoperative planning, especially in patients where intraoperative navigation may not be available.
Conclusion
Based on the findings from our studies and the collective conclusion of previous studies, the placement of Transpedicular, translaminar, and LMS in the sub-axial cervical vertebrae in the Iranian population may be appropriate. The results concluded that most of the parameters were highest at C7, which includes the OPH, OPW, IPH, IPW, PAL, translaminar thickness, translaminar height, translaminar sagittal diagonal thickness, translaminar length, and lateral mass diagonal height.
On the other hand, the PTA parameter was noted to be highest at C5. Lateral mass parameters at depth, coronal width, lateral angulation, and coronal height were the highest at C3. The lateral mass axial width parameter was the widest at C6, and the Lateral mass sagittal thickness had the highest value at C4.
Limitations
This study was limited by its retrospective design and the relatively small sample size, which may not fully represent the broader Iranian population. Additionally, only CT images from one center were used, and there was no intra-observer or interobserver reliability assessment for the measurements.
Ethical Considerations
Compliance with ethical guidelines
The data was collected anonymously from the Rajaie Hospital’s PACS program and kept confidential throughout. The study has been approved by the Ethics Committee of Qazvin University of Medical Sciences, Qazvin, Iran (Code: IR.QUMS.REC.1398.294).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Sina Abdollahzade; Data collection: Yasaman Ghiasi;
Data analysis and interpretation: Sina Abdollahzade, Yong Yie Liew, and Arup Ray; Writing the original draft and final approval: All authors; Review and editing: Sina Abdollahzade, Yasaman Ghiasi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to express their sincere gratitude to Rajayee Hospital for its valuable support and contribution to this work.
References
The stability of the cervical spine can be affected by multitudes of pathologies, including, but not limited to, trauma, malformations, tumors, and osteoarthritis. An unstable cervical spine might mandate surgical intervention in the form of stabilization and fusion. To stabilize the cervical spine, surgeons have used different methods and devices through the posterior approach. These procedures are commonly undertaken for pathologies affecting sub-axial cervical vertebrae [1-5].
Most spinal surgeons use lateral mass screws (LMS) for sub-axial cervical vertebrae stabilization, as it provides excellent stability whilst maintaining a high fusion rate [6-8]. LMS has been associated with loosening or erosion, which may require further fixation of the screws into the pedicle [9, 10]. Laminar screws are also increasingly used in the treatment of cervical pathologies [11].
The most reliable technique for stabilizing the spine is transpedicular screw fixation (TPSF) [12, 13]. However, it presents a unique challenge in the cervical region due to the proximity of the pedicles to eloquent structures, such as vertebral arteries, spinal cord, and nerve roots. The complexity of cervical spine anatomy is due to pedicle dimension and angulation variations among various ethnicities and proximity to vital neurovascular structures [14, 15]. A thorough understanding of the morphometric features of the cervical spine is essential for any spine surgeon dealing with it and crucial for implant design and development [16-18]. Pedicle screws provide higher biomechanical stability, while LMS are more straightforward to place [19, 20]. These, along with laminar screws, are key parts of any spine surgeon’s toolkit to deal with this complex region of the spinal column through a posterior approach.
A good understanding of the cervical anatomy is required for successful insertion of any type of screw to avoid damage to nearby elements, such as spinal cord injury, durotomy, vascular injury, and inadequate bone purchase that may predispose the implant to loosening, pull out, and eventual failure [14, 21]. Before any surgical interventions, surgeons will evaluate the anatomy of the vertebrae using a computed tomography (CT) scan to determine the size, shape, and angle of the pedicle. This is increasingly important for the management of deformity cases where the characteristics of a normal spinal anatomy are probably deranged [22].
Studies have shown that there are significant differences in terms of morphometric measurements between races and genders, emphasizing the importance of studying the morphometry of the vertebrae in different populations to increase the safety and accuracy of surgery [23]. Despite existing data from other ethnic groups, there is limited information on the morphometry of the cervical spine in the Iranian population. These anatomical variations are critical for safe screw placement in spinal surgery. This is especially important in Iran, where spinal screws are mostly not locally manufactured and are imported, often based on foreign anatomical standards. Therefore, this study evaluates the feasibility of transpedicular, translaminar, and lateral mass screw placement by assessing morphometric characteristics in a representative Iranian sample using CT imaging, to evaluate the differences between the existing screws and actual population cervical spinal morphometry.
Methods and Materials/Patients
Study design
This was a cross-sectional, retrospective morphometric study conducted on CT images obtained from Rajaei Hospital, Qazvin, Iran, PACS records.
The simple random sampling was used to select 100 CT scans from adult patients who met the inclusion criteria. Cervical CT scan imaging of 100 adult patients (above 18 on enrolment day) who underwent CT imaging for various clinical reasons (e.g. trauma) and were referred to Rajaei Hospital in Qazvin City, Iran, was retrospectively reviewed in this cross-sectional study. The exclusion criteria were as follows: 1) Non-standard and low-quality CT scan; 2) Vertebral fracture; 3) Pre-existing pathologies of the cervical spine, including infection, rheumatoid arthritis, or masses in the vertebrae; 4) History of surgery on the spine; and 5) Ankylosing spondylitis.
Measurements including the length, width, height, and placement angles of the three types of screws (transpedicular, translaminar, and lateral mass) of the subaxial cervical vertebrae were obtained from the cervical CT imaging.
Data collection
A checklist including age, sex, and measured parameters of the vertebrae was completed by the study manager, and the measurements were performed on the CT scan images using the Marco PACS division program (last version: 14.29.55).
The parameters were measured on CT scan slices where their values were at their maximum, and the values were expressed in millimeters. The measured parameters are shown in the following figures (Figures 1, 2, and 3).
Statistical analysis
The collected data were entered into the computer using the SPSS software, version 19 (developed by IBM, version: 28.0.1). For descriptive results, the frequency, Mean±SD were calculated based on the type of the variables. The results were analyzed using an independent t-test and a chi-square test to examine the relationship between quantitative and qualitative variables. Meanwhile, a P<0.05 was considered significant.
Results
Baseline characteristics
In this study, the length, width, height, and placement angles of the three types of screws (translaminar, transpedicular, and lateral mass) of the subaxial cervical vertebrae of 100 patients were examined. A total of 58 patients (58%) were male and 42 patients (42%) were female. The mean age of the patients was 37.4±12.7 years and ranged from 18 to 67 years. Before examining the objectives, the distribution of data was checked in terms of normality using the Kolmogorov–Smirnov test, and the normal results were confirmed. The results of the study objectives were obtained in the following tables.
Mean outer pedicle height (OPH) on CT scan: The mean outer height of the pedicle isthmus was greatest at C7 and applied to both left and right. Mean outer pedicle width (OPW) in CT scan: The mean outer width of the pedicle isthmus was greatest at C7 and applied to both left and right.
Mean inner pedicle height (IPH) on CT scan: The mean inner height of the pedicle isthmus was greatest at C7 and applied to both left and right.
Mean inner pedicle width (IPW) on CT scan: The mean inner width of the pedicle isthmus was greatest at C7 and applied to both left and right.
Mean pedicle axis length (PAL) on CT scan: The mean distance from the posterior point of the pedicle axis on the lateral mass to the anterior margin of the vertebral body was greatest at C7 and was almost greater on the right side than on the left.
Mean pedicle transverse angle (PTA) on CT scan: The mean angle between the pedicle axis and the anatomical sagittal plane was greatest at C4 and C5 on the right side (Table 1).
Mean translaminar length on CT scan: The mean translaminar length from the junction of the lateral mass and the lamina to the outer layer opposite the spinous process was greatest at C7 and was similar on the right and left sides. The average was higher at C3 on the left and C6 on the right.
Mean translaminar thickness on CT scan: The mean thickness or maximum distance from ventromedial to dorsolateral portions of the centre of the lamina was greatest at C7 and greater on the right side.
Mean translaminar height on CT scan: The mean maximum height between the spinous process and the base of the pedicle was greatest at C7 and was almost identical on the right and left sides.
Mean translaminar sagittal diagonal thickness on CT scan: The mean sagittal oblique distance from the most head point of the lamina to the tail end of it was greatest at C7 and was almost greater on the right side (Table 2).
Mean lateral mass axial depth on CT scan: The mean anterior-posterior distance in the sagittal cut was greatest at C3 and almost greater on the right side.
Mean lateral mass axial width on CT scan: The mean internal-external distance in the sagittal cut was greatest at C6 and almost greater on the left side.
Mean lateral mass lateral angulation on CT scan: The mean medial distance above the centre of the lateral mass was greatest in C3 and was similar on the right and left sides.
Mean lateral mass sagittal thickness on CT scan: The mean thickness from the dorsal area to the ventral from the centre of the lateral mass was greatest at C7 and was almost greater on the left side.
Mean lateral mass diagonal height on CT scan: The mean distance from the tip of the superior articular facet to the inferior articular facet was greatest at C7 and greater on the right side.
Mean lateral mass coronal height on CT scan: The mean height of the head-to-tail distance from the centre of the lateral mass was greatest at C3 in the coronal cut and was greater on the right side.
Mean lateral mass coronal width on CT scan: The mean width of the internal-external distance in the coronal cut was greatest in C7 and was greater on the left side (Table 3).
Discussion
Overview of morphometric findings
Cervical fixation has been increasingly used in posterior approaches of the subaxial cervical region for multiple pathologies, and various techniques are utilized for this purpose, including lateral mass, pedicular, and translaminar screws. As the morphology of this complex region can be inconsistent among different ethnic groups, in the present study, the feasibility of inserting transpedicular, translaminar, and LMS was evaluated in the Iranian population.
This study demonstrates that the OPH, OPW, IPH, and IPW were measured to be highest at C7. The mean values of IPH and IPW were noted to be 3.5 mm and 3.4 mm, respectively, at C7. Whilst the mean IPH and IPW parameters were 3.5 mm at C7. Based on the findings of a review study by Liu et al., the mean OPW of the sub-axial spine in Asians was between 5.26-6.63 mm, and was between 5.17-6.64 mm in Europe/America [24].
Comparison with other populations
In a study by Al-Saeed et al., this morphometric parameter (OPW) had a mean of 5.8 mm at C7 in the Arab population [18]. These studies are consistent with the findings of the present study. In a 2014 study by Wasinpongwanich et al., OPH and OPW parameters were suitable for all sub-axial cervical spines with 3.5 mm screw placement [25].
In a recent study by Farooque et al. In 2018, CT scan results of 500 sub-axial cervical spines per 100 patients showed that the mean PW had the lowest value at C3 (4.3 mm) and highest at C7 (5.7 mm), which is coherent with the results of the present study. The study also showed that the mean PH had the lowest value at C3 (5.5 mm) and the highest at C7 (6.1 mm) [26], whilst in our study, C5 had the lowest mean IPW (OPW had the same mean value at C3, C5, and C6), and C7 had the highest mean IPW and OPW.
In a recent study by Alsaleh et al. In 2021, CT scan results in 207 patients suggested that the mean PW ranged from 4.4 mm at C3 to 6.1 mm at C7, and the mean PH ranged from 6.4 mm at C3 to 6.8 mm at C7 [27]. In the present analysis, mean OPW ranged from 5.2 mm at C3 to 6.5 mm at C7, and the mean OPH ranged from 6.6 mm at C3 to 6.9 mm at C7.
According to the present results, the PAL parameter had the highest value with a mean of 31.3 mm at C7. These findings are supported by Farooque et al. (2018), which showed that the mean PAL parameter was lowest at C3 (29.6 mm) and highest at C7 (33.04 mm) [26].
Measurements revealed that the PTA parameter, with an average of 42.1˚ had the highest value at C5. These parameters were similar on the left and right sides. This is in keeping with the findings from Chazono et al., which reported that the PTA was measured to be 37.1-49 degrees in the sub-axial spine in the Asian population and 38.7-48.8 degrees in the European/American population [9]. In the 2014 study by Wasinpongwanich et al., the results indicated that the PTA parameter had the highest value at C5 and the lowest value at C7, and the measurements were similar on both the left and right side [25]. In the study by Farooque et al. (2018), the mean PTA parameter was highest at C3 (44.58°) and lowest at C7 (37.18°) [26]. The data were comparable to the findings by Alsaleh et al. in 2021 [27]. Their study was able to show a varying mean PTA parameter of 42 to 51 degrees between different levels of C1-C7.
Although the pedicle width and height measurements of the Iranian population in our study were largely comparable to those reported in Arab, East Asian, and Western populations, subtle but clinically relevant differences were observed. For example, the mean OPW at C7 in our study was approximately 6.5 mm, compared to 5.8 mm in Arab populations and up to 6.6 mm in East Asian studies. This 0.5–0.7 mm variation may appear minor, but considering that cervical pedicle screws typically measure 3.5 mm in diameter, such differences can significantly influence the decision to proceed with pedicle screw placement. A narrower pedicle increases the risk of cortical wall violation, which potentially leads to neurovascular complications. These findings indicate the importance of obtaining population-specific morphometric data to guide preoperative planning, particularly in regions where generic or Western anatomical data are often used by default.
Translaminar morphometry
This study suggested that the thickness, height, and sagittal diagonal of the translaminar parameter were measured to have an average of 6.14, 10.37, and 18.97 mm at C7, respectively. On the other hand, the translaminar length parameter was averaged to be 20.65 mm at C3 and had the highest value at C7 (20.85 mm). Comparatively, in a study in 2015 by Ji et al., thickness, height, and diagonal- sagittal measurements of translaminar screw placement and feasibility analysis using one-sided and two-sided placement of 3.5 mm cervical screws on CT scan was assessed in 0.5 mm distance from the safety margin and the results showed that the translaminar length parameter with a maximum mean of 21.8 mm, the thickness parameter with an average of 6.1 mm, the height parameter with an average of 10.8 mm and the sagittal diagonal parameter with an average of 19.8 mm at C7 had the highest value [28]. The findings of the present study are in line with the study of Ji et al.
Lateral mass morphometry
Analysis of the data revealed that the depth and height of the lateral mass were highest at C3 with average values of 11.96 and 13.58 mm, respectively, and the axial width was noted to have an average of 12.69 mm at C6. In 2018, Patil et al. carried out a study on 104 patients in India to measure the lateral sub-axial cervical spine using axial, sagittal, and coronal CT scans, as well as anteroposterior and lateral x-rays. The results showed that the lateral masses were thinner and longer descending from C3 to C7 [29].
The results of the current study showed that the lateral mass parameters in lateral angulation and coronal height had the highest values at C3, with an average of 54.61 and 13.58 mm, respectively. In the study by Patil et al., they depicted that the lateral angulation was highest at C6 (24.4°) and lowest at C3 (22.7°). The coronal height parameter was measured to be the highest at C3, with an average of 12.9 mm [29].
According to the other findings of this study, the lateral mass sagittal thickness had the highest average value at C4 (11.95 mm), whilst the coronal width had the highest value at C3, averaging 10.79 mm and the lateral mass diagonal height had the highest value at C7 (24.08 mm). In the study by Patil et al., the sagittal incision thickness and the oblique length increased from C3 to C7. In their study, the sagittal incision thickness of 18 mm, and diagonal height parameter of 22.8 mm, and the coronal width parameter of 12.4 mm in C7 had the highest value [29].
Clinical implications
Based on the morphometric data, pedicle screw placement appears most feasible at the C7 level due to wider pedicle dimensions (OPW/IPW ~6.5/3.5 mm), which allows the surgeon to safely insert 3.5 mm screws with acceptable margins. At higher levels, such as C3–C5, where pedicle dimensions are narrower, lateral mass or translaminar screws are likely safer and preferable. The observed PTA values (up to ~42° at C5) provide intraoperative guidance for angulation to avoid cortical breaches. These data can help neurosurgeons in preoperative planning, especially in patients where intraoperative navigation may not be available.
Conclusion
Based on the findings from our studies and the collective conclusion of previous studies, the placement of Transpedicular, translaminar, and LMS in the sub-axial cervical vertebrae in the Iranian population may be appropriate. The results concluded that most of the parameters were highest at C7, which includes the OPH, OPW, IPH, IPW, PAL, translaminar thickness, translaminar height, translaminar sagittal diagonal thickness, translaminar length, and lateral mass diagonal height.
On the other hand, the PTA parameter was noted to be highest at C5. Lateral mass parameters at depth, coronal width, lateral angulation, and coronal height were the highest at C3. The lateral mass axial width parameter was the widest at C6, and the Lateral mass sagittal thickness had the highest value at C4.
Limitations
This study was limited by its retrospective design and the relatively small sample size, which may not fully represent the broader Iranian population. Additionally, only CT images from one center were used, and there was no intra-observer or interobserver reliability assessment for the measurements.
Ethical Considerations
Compliance with ethical guidelines
The data was collected anonymously from the Rajaie Hospital’s PACS program and kept confidential throughout. The study has been approved by the Ethics Committee of Qazvin University of Medical Sciences, Qazvin, Iran (Code: IR.QUMS.REC.1398.294).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Sina Abdollahzade; Data collection: Yasaman Ghiasi;
Data analysis and interpretation: Sina Abdollahzade, Yong Yie Liew, and Arup Ray; Writing the original draft and final approval: All authors; Review and editing: Sina Abdollahzade, Yasaman Ghiasi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to express their sincere gratitude to Rajayee Hospital for its valuable support and contribution to this work.
References
- Ilgenfritz RM, Gandhi AA, Fredericks DC, Grosland NM, Smucker JD. Considerations for the use of C7 crossing laminar screws in subaxial and cervicothoracic instrumentation. Spine. 2013; 38(4):E199-204. [DOI:10.1097/BRS.0b013e31827de094] [PMID]
- Hong JT, Sung JH, Son BC, Lee SW, Park CK. Significance of laminar screw fixation in the subaxial cervical spine. Spine. 2008; 33(16):1739-43. [DOI:10.1097/BRS.0b013e31817d2aa2] [PMID]
- Pateder DB, Carbone JJ. Lateral mass screw fixation for cervical spine trauma: Associated complications and efficacy in maintaining alignment. Spine Journal. 2006; 6(1):40-3. [DOI:10.1016/j.spinee.2005.04.010] [PMID]
- Sciubba DM, Noggle JC, Vellimana AK, Conway JE, Kretzer RM, Long DM, et al. Laminar screw fixation of the axis. Journal of neurosurgery. Spine. 2008; 8(4):327-34. [DOI:10.3171/SPI/2008/8/4/327] [PMID]
- Şenoğlu M, Özkan F, Çelik M. Placement of C-7 intralaminar screws: A quantitative anatomical and morphometric evaluation. Journal of Neurosurgery. Spine. 2012; 16(5):509-12. [DOI:10.3171/2012.1.SPINE111048] [PMID]
- Abuzayed B, Tutunculer B, Kucukyuruk B, Tuzgen S. Anatomic basis of anterior and posterior instrumentation of the spine: Morphometric study. Surgical and Radiologic Anatomy. 2010; 32(1):75-85. [DOI:10.1007/s00276-009-0545-4] [PMID]
- Nakanishi K, Tanaka M, Sugimoto Y, Misawa H, Takigawa T, Fujiwara K, et al. Application of laminar screws to posterior fusion of cervical spine: Measurement of the cervical vertebral arch diameter with a navigation system. Spine. 2008; 33(6):620-3. [DOI:10.1097/BRS.0b013e318166aa76] [PMID]
- Alvin MD, Abdullah KG, Steinmetz MP, Lubelski D, Nowacki AS, Benzel EC, et al. Translaminar screw fixation in the subaxial cervical spine: Quantitative laminar analysis and feasibility of unilateral and bilateral translaminar virtual screw placement. Spine. 2012; 37(12):E745-51. [DOI:10.1097/BRS.0b013e31824c70ef] [PMID]
- Chazono M, Tanaka T, Kumagae Y, Sai T, Marumo K. Ethnic differences in pedicle and bony spinal canal dimensions calculated from computed tomography of the cervical spine: A review of the English-language literature. European Spine Journal. 2012; 21(8):1451-8. [DOI:10.1007/s00586-012-2295-y] [PMID] [PMCID]
- Kayalioglu G, Erturk M, Varol T, Cezayirli E. Morphometry of the cervical vertebral pedicles as a guide for transpedicular screw fixation. Neurologia Medico-Chirurgica. 2007; 47(3):102-7. [DOI:10.2176/nmc.47.102] [PMID]
- Yusof MI, Ming LK, Abdullah MS. Computed tomographic measurement of cervical pedicles for transpedicular fixation in a Malay population. Journal of Orthopaedic Surgery. 2007; 15(2):187-90. [DOI:10.1177/230949900701500213] [PMID]
- Jea A, Sheth RN, Vanni S, Green BA, Levi AD. Modification of Wright’s technique for placement of bilateral crossing C2 translaminar screws: Technical note. Spine Journal. 2008; 8(4):656-60. [DOI:10.1016/j.spinee.2007.06.008] [PMID]
- Kretzer RM, Chaput C, Sciubba DM, Garonzik IM, Jallo GI, McAfee PC, et al. A computed tomography-based feasibility study of translaminar screw fixation in the upper thoracic spine. Journal of Neurosurgery. Spine. 2010; 12(3):286-92. [DOI:10.3171/2009.10.SPINE09546] [PMID]
- Tarawneh AM, Haleem S, D'Aquino D, Quraishi N. The comparative accuracy and safety of fluoroscopic and navigation-based techniques in cervical pedicle screw fixation: Systematic review and meta-analysis. Journal of Neurosurgery. Spine. 2021; 35(2):194-201. [DOI:10.3171/2020.11.SPINE201877] [PMID]
- Chachan S, Bin Abd Razak HR, Loo WL, Allen JC, Shree Kumar D. Cervical pedicle screw instrumentation is more reliable with O-arm-based 3D navigation: analysis of cervical pedicle screw placement accuracy with O-arm-based 3D navigation. European Spine Journal. 2018; 27(11):2729-36. [DOI:10.1007/s00586-018-5585-1] [PMID]
- Mao GP, Zhao JN, Wang YR, Li JS, Chen YX, Wu SJ, et al. Design of cervical pedicle locator and three-dimensional location of cervical pedicle. Spine. 2005; 30(9):1045-50. [DOI:10.1097/01.brs.0000161011.08086.5b] [PMID]
- Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: A meta-analysis. Spine. 2007; 32(3):E111-20. [DOI:10.1097/01.brs.0000254048.79024.8b] [PMID]
- Al-Saeed O, Marwan Y, Kombar OR, Samir A, Sheikh M. The feasibility of transpedicular screw fixation of the subaxial cervical spine in the Arab population: A computed tomography-based morphometric study. Journal of Orthopaedics and Traumatology. 2016; 17(3):231-8. [DOI:10.1007/s10195-016-0396-9] [PMID] [PMCID]
- Kotil K, Akçetin MA, Savas Y. Neurovascular complications of cervical pedicle screw fixation. Journal of Clinical Neuroscience. 2012; 19(4):546-51. [DOI:10.1016/j.jocn.2011.05.041] [PMID]
- Nakashima H, Yukawa Y, Imagama S, Kanemura T, Kamiya M, Yanase M, et al. Complications of cervical pedicle screw fixation for nontraumatic lesions: A multicenter study of 84 patients. Journal of Neurosurgery. Spine. 2012; 16(3):238-47. [DOI:10.3171/2011.11.SPINE11102] [PMID]
- Cheung JP, Luk KD. Complications of anterior and posterior cervical spine surgery. Asian Spine Journal. 2016; 10(2):385-400. [DOI:10.4184/asj.2016.10.2.385] [PMID] [PMCID]
- Rajasekaran S, Vaccaro AR, Kanna RM, Schroeder GD, Oner FC, Vialle L, et al. The value of CT and MRI in the classification and surgical decision-making among spine surgeons in thoracolumbar spinal injuries. European Spine Journal. 2017; 26(5):1463-9. [DOI:10.1007/s00586-016-4623-0] [PMID]
- Kretzer RM, Hu N, Kikkawa J, Garonzik IM, Jallo GI, Tortolani PJ, et al. Surgical management of two-versus three-column injuries of the cervicothoracic junction: Biomechanical comparison of translaminar screw and pedicle screw fixation using a cadaveric model. Spine. 2010; 35(19):948-54. [DOI:10.1097/BRS.0b013e3181c9f56c] [PMID]
- Liu J, Napolitano JT, Ebraheim NA. Systematic review of cervical pedicle dimensions and projections. Spine. 2010; 35(24):1373-80. [DOI:10.1097/BRS.0b013e3181e92272] [PMID]
- Wasinpongwanich K, Paholpak P, Tuamsuk P, Sirichativapee W, Wisanuyotin T, Kosuwon W, et al. Morphological study of subaxial cervical pedicles by using three-dimensional computed tomography reconstruction image. Neurologia Medico-Chirurgica. 2014; 54(9):736-45. [DOI:10.2176/nmc.oa.2013-0287] [PMID] [PMCID]
- Farooque K, Yadav R, Chowdhury B, Gamanagatti S, Kumar A, Meena PK. Computerized tomography-based morphometric analysis of subaxial cervical spine pedicle in asymptomatic Indian population. International Journal of Spine Surgery. 2018; 12(2):112-20. [DOI:10.14444/5017] [PMID] [PMCID]
- Alsaleh K, Essbaiheen F, Aldosari K, Alsubei B, Alabdulkareeem M. Morphometric analysis of subaxial cervical spine pedicles in a middle Eastern population. International Journal of Spine Surgery. 2021; 15(3):413-7. [DOI:10.14444/8061] [PMID] [PMCID]
- Ji GY, Oh CH, Park SH, Kurniawan F, Lee J, Jeon JK, et al. Feasibility of translaminar screw placement in Korean population: Morphometric analysis of cervical spine. Yonsei Medical Journal. 2015; 56(1):159-66. [DOI:10.3349/ymj.2015.56.1.159] [PMID] [PMCID]
- Patil ND, Srivastava SK, Bhosale S, Purohit S. Computed tomography-and radiography-based morphometric analysis of the lateral mass of the subaxial cervical spine in the Indian population. Asian Spine Journal. 2018; 12(1):18-28. [DOI:10.4184/asj.2018.12.1.18] [PMID] [PMCID]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |