Wed, Feb 4, 2026
Volume 10 - Continuous Publishing
Iran J Neurosurg 2024, 10 - Continuous Publishing: 49-55 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Akbulut B B, Biçeroğlu H, Akalın T, Bölük M S, Yurtseven T. Thoracolumbar Paravertebral Intramuscular Myxoma Presenting with Mechanical Back Pain: A Case Report and Review of the Literature. Iran J Neurosurg 2024; 10 : 5
URL: http://irjns.org/article-1-405-en.html
URL: http://irjns.org/article-1-405-en.html
Bilal Bahadır Akbulut *1 

 , Hüseyin Biçeroğlu2
, Hüseyin Biçeroğlu2 

 , Taner Akalın3
, Taner Akalın3 

 , Mustafa Serdar Bölük2
, Mustafa Serdar Bölük2 

 , Taşkın Yurtseven2
, Taşkın Yurtseven2 




 , Hüseyin Biçeroğlu2
, Hüseyin Biçeroğlu2 

 , Taner Akalın3
, Taner Akalın3 

 , Mustafa Serdar Bölük2
, Mustafa Serdar Bölük2 

 , Taşkın Yurtseven2
, Taşkın Yurtseven2 


1- Department of Neurosurgery, Faculty of Medicine, Ege University, Izmir, Turkey. , b.bahadirakbulut@gmail.com
2- Department of Neurosurgery, Faculty of Medicine, Ege University, Izmir, Turkey.
3- Department of Pathology, Faculty of Medicine, Ege University, Izmir, Turkey.
2- Department of Neurosurgery, Faculty of Medicine, Ege University, Izmir, Turkey.
3- Department of Pathology, Faculty of Medicine, Ege University, Izmir, Turkey.
Full Text [PDF 5428 kb]
(932 Downloads)
| Abstract (HTML) (3415 Views)
Full Text: (678 Views)
1. Background and Importance
Myxomas are mesenchymal tumors that are benign and are mainly found in cardiac tissues but are seldom ob-served in skeletal muscle tissues. Paraspinal intramuscular myxoma is even more of a rarity with limited studies that discuss clinical manifestations, diagnostic criteria, and treatment options [1–5]. Arising out of fibroblasts that are known to overproduce the mucinous extracellular matrix, these tumors are mostly of non-aggressive behavior but are a major diagnostic and therapeutic dilemma due to their anatomical location and the similari-ties in the presentation with other spindle cell neoplasms [6].
The rarity of paraspinal intramuscular myxomas and the critical anatomical relationship of the paraspinal region with the spinal structures only worsen the need for extensive research since the small number of documented cases does not allow for evidence-based clinical guidelines.
In this paper, we present an in-depth discussion of a case of intramuscular myxoma situated in the lumbar paraspinal musculature and a literature review of this rare entity.
2. Case Presentation
The case of this study was a 46-year-old female who presented with back pain exacerbating with movement over 3 months. A thoracolumbar magnetic resonance imaging (MRI) was performed (Figure 1), revealing a T2 hyperintense 35×25×85 mm mass that extends craniocaudally within the right-sided paraspinal muscles corresponding to the T11-L1 levels. There was heterogeneous contrast enhancement on T1 sequence images. Subsequent CT imaging revealed the lesion to be non-contrast enhancing and hypodense. Radiology suggested a myxoma or an abscess within the paraspinal musculature. Acute phase reactants were within normal levels, with CRP of 1 and WBC of 6.91. The mass within the paraspinal musculature can be visualized and palpated during the physical examination. The patient had no neurological symptoms.
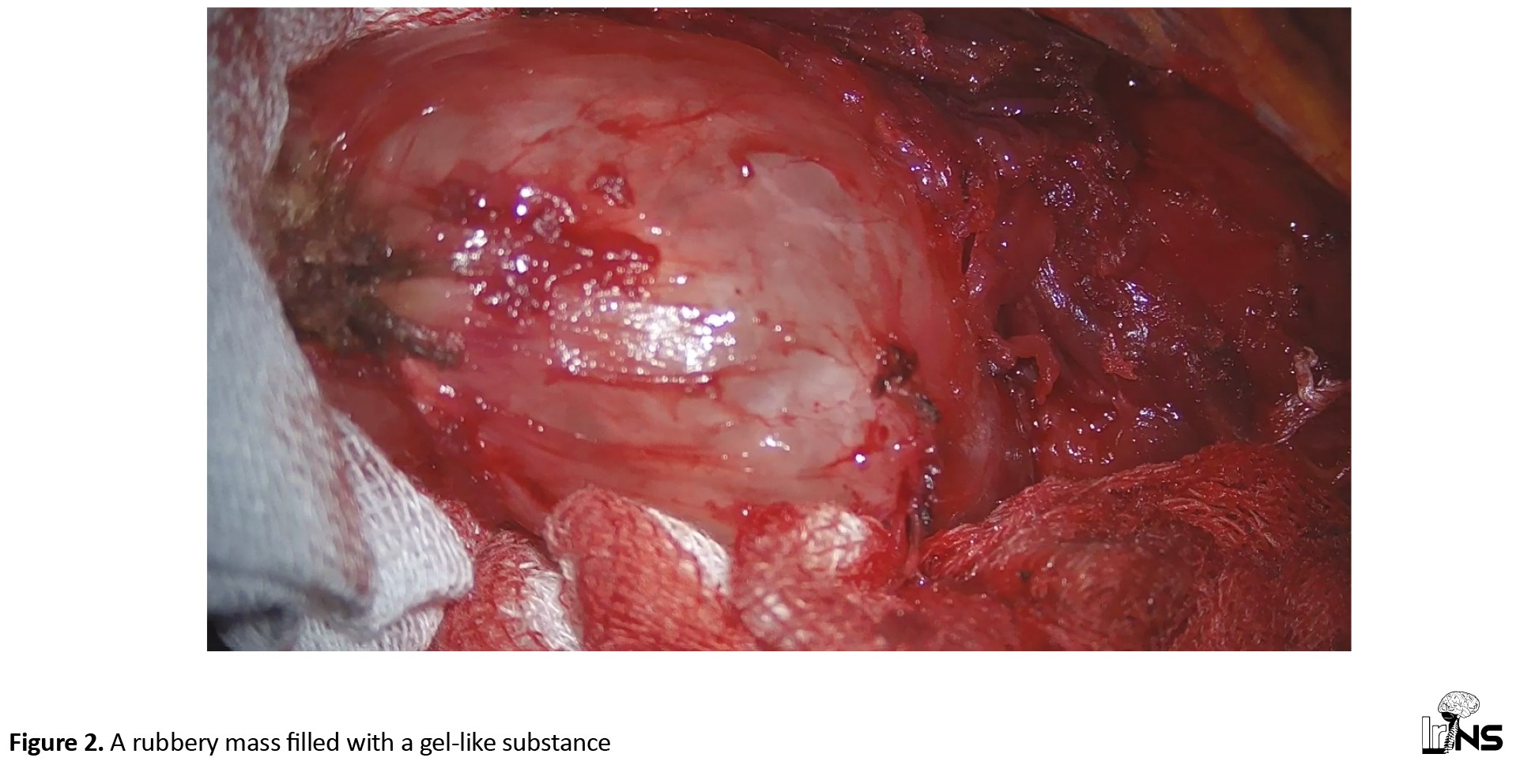
The patient was operated under general anesthesia using a paramedian incision, paraspinal muscles were dissected and a rubbery mass was palpated within (Figure 2). The tumor was mobilized in all quadrants and removed with a 1 cm margin within the paraspinal muscles. The tumor had a gel-like internal substance. There was no complication intraoperatively and the wound was closed.
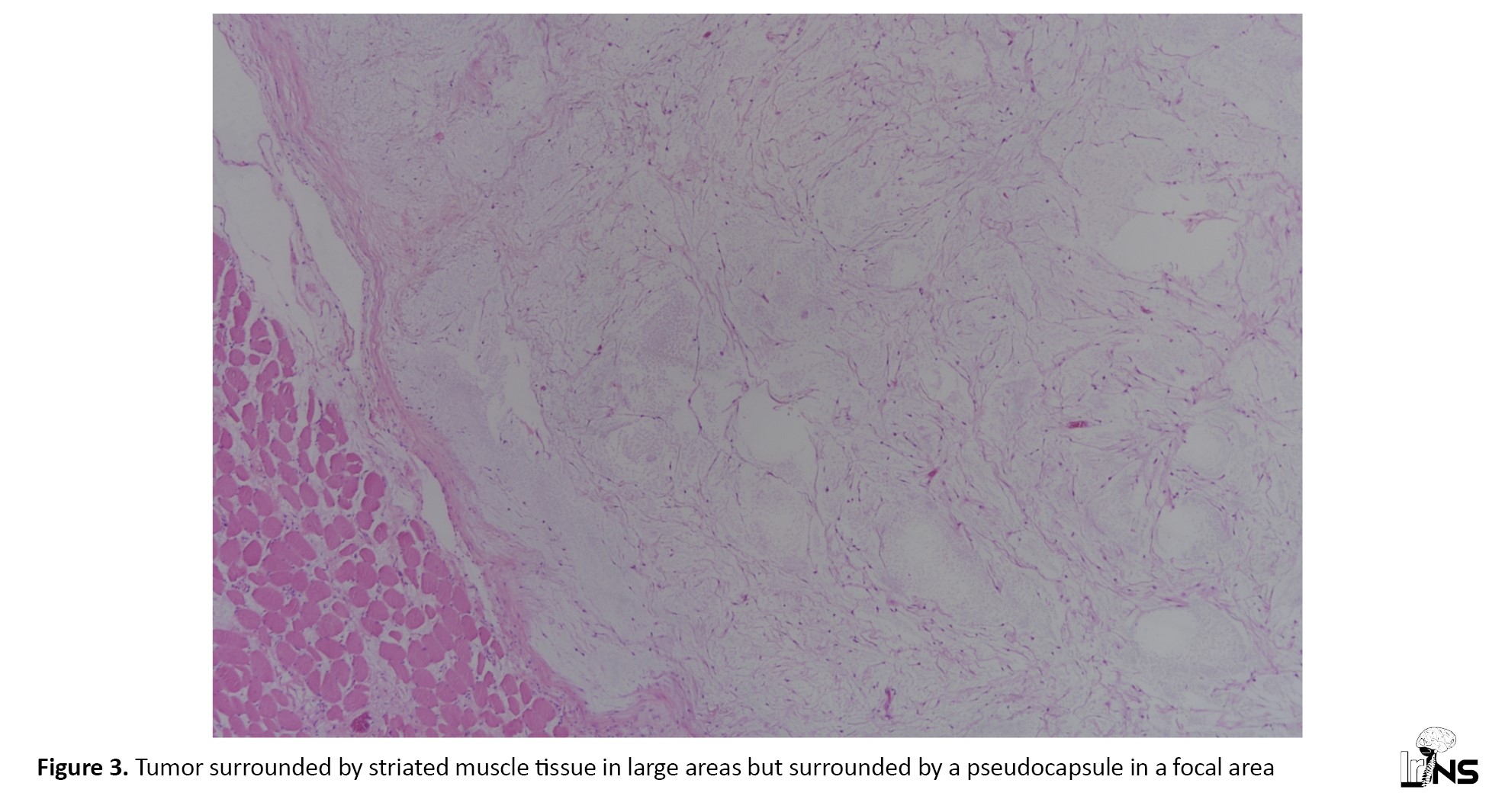
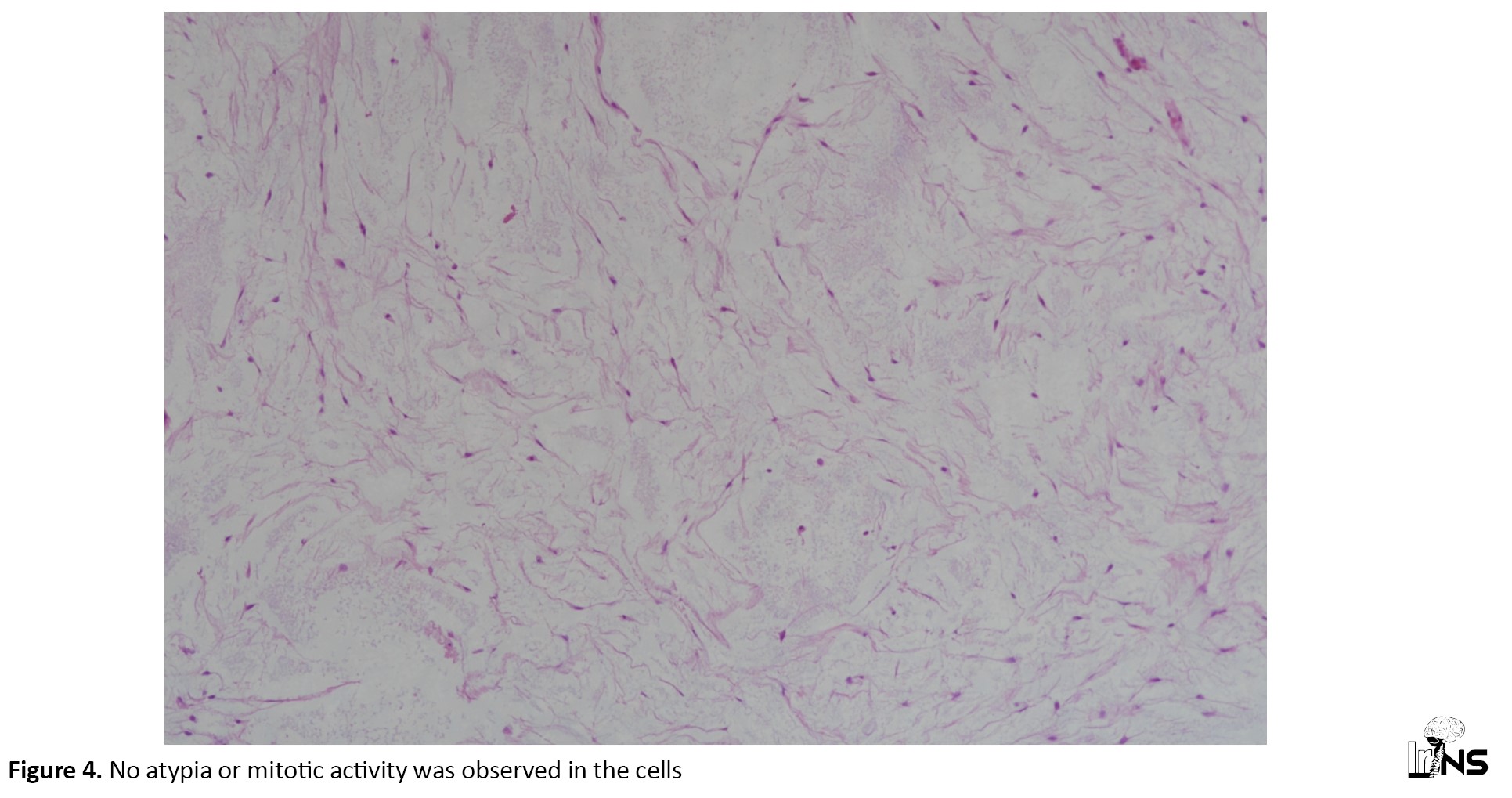
Histopathological examination revealed a tumor characterized by a loose arrangement of spindle-stellated cells on a distinct myxoid background. The tumor was surrounded by striated muscle tissue in large areas but was surrounded by a pseudocapsule in a focal area (Figure 3). No atypia or mitotic activity was observed in the cells (Figure 4). Immunohistological staining was focally positive for CD34 and smooth muscle actin but negative for desmin, S-100, MUC4, and SOX-10 protein. The tumor had a Ki67 of 1%.
The postoperative MRI scan revealed complete removal of the tumor and the patient was followed up for 2 days and discharged without complications.
3. Literature Review
Materials and Methods
A PubMed search was performed using “(intramuscular) AND (myxoma)” keywords in the PubMed-National Center for Biotechnology Information database. Two-hundred and sixty studies were found published before October 2023. Out of these, 18 papers were relevant, 14 of which were in English and had an available full-text (Figure 5).
4. Results
A total of 14 studies are included in this review, comprising 16 cases, including this case report (Table 1).
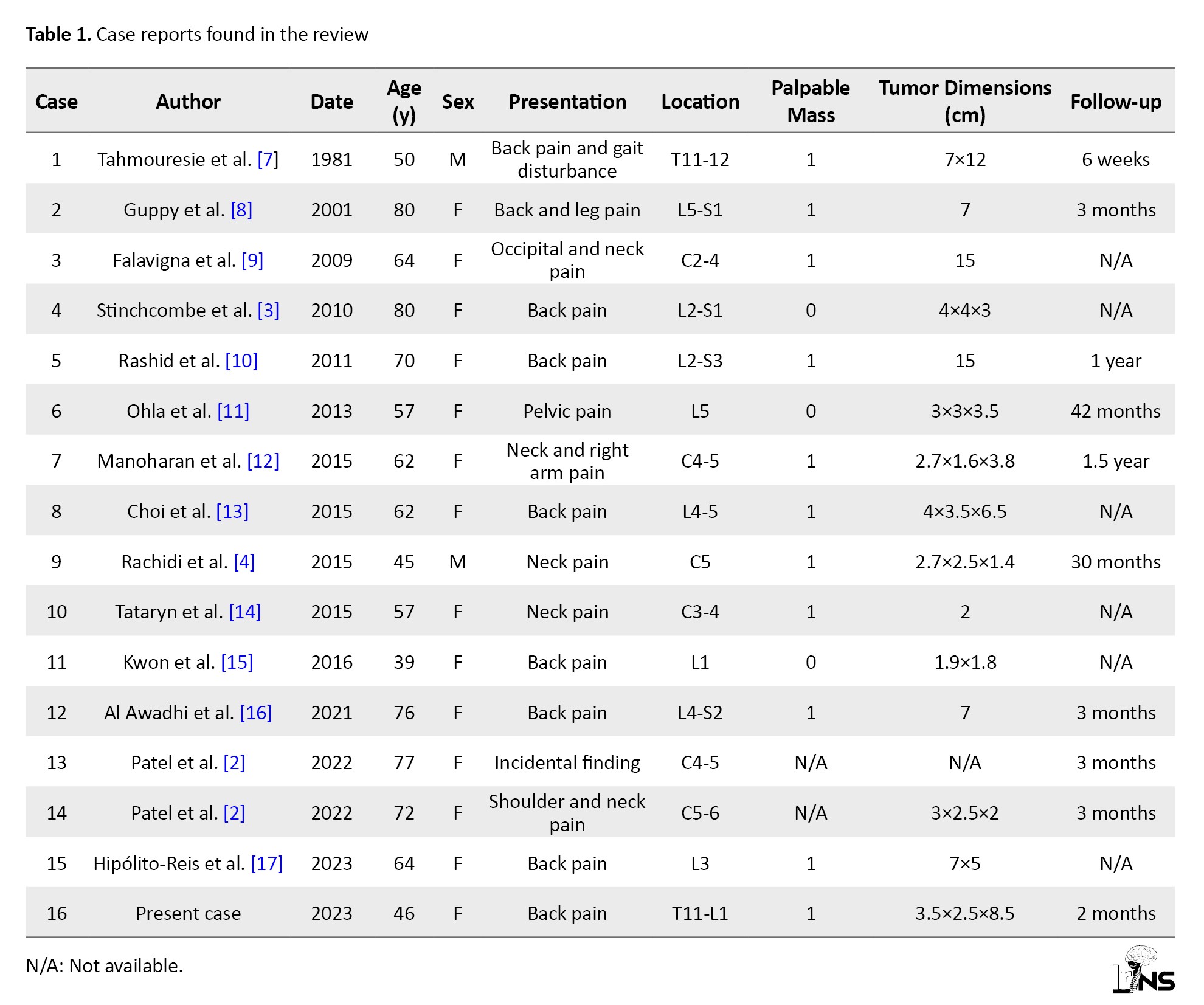
Median age was 63 (range 39-80), with female predominance (n=14, 87.5%). Most of the cases were located in the thoracolumbar area (n=10, 62.5%). Of the cases available, 78% had a palpable mass on presentation (n=11).
5. Discussion
Intramuscular myxomas are a rare paraspinal musculature pathology. As far as we know there have been 16 cases, including our present case.
This pathology most commonly presents as back pain, with radicular pain in cases of spinal canal involvement. Treatment paradigms are mainly centered on surgical resection for extramarginal resection with or without neurological function preservation as appropriate. The literature mirrors positive results with surgical treatment, in most cases with low rates of recurrence.
Back pain is a very common issue that has a 1-year incidence of any episode of low back pain ranging between 1.5% and 36% [18], which increases with age, up to the age of 60-65. In the literature, 78% (n=11) of the cases had a palpable mass on presentation, showing us how important it is to palpate the patient’s back and physically examine for any masses or signs that might explain the pain and might provide an early diagnosis.
The histopathological diagnosis of myxoma is mainly identified by myxoid stroma containing loose, stellate, or spindle-shaped cells with ill-defined outlines and a minimal amount of eosinophilic cytoplasm. The characteristic myxoid stroma is rich in hyaluronic acid and other mucopolysaccharides, giving the tumor a loose or gelatinous texture. The vascular pattern in myxomas often reveals poorly developed capillary-like vessels with sparse and thin walls. The cells’ nuclei are usually small, unremarkable, and lack significant pleomorphism or mitotic activity, a sign of a benign character. Immunohistochemical analysis is ancillary, vimentin is positive, and desmin and S100 protein are typically negative. The myxoid matrix is further enhanced by special staining procedures, especially Alcian blue which binds to mucopolysaccharides and helps distinguish the myxomas from other soft tissue tumors. The precise histological evaluation, combined with immunohistochemical staining, and probably molecular analyses, constitute the cornerstone for the definitive diagnosis of myxoma, differentiating it from other myxoid or spindle cell neoplasms in the differential diagnosis [19].
6. Conclusion
Myxomas in the paraspinal region are rare but important intramuscular tumors due to their propensity to mimic common back pain, requiring inclusion in the differential diagnoses. The total excision of the tumor, as was the case in this patient, led to symptom relief and a low risk of recurrence, highlighting surgery as the treatment of choice.
The accumulation of 16 documented cases, including this one, adds to the knowledge of paraspinal intramuscular myxomas with a female predominance and frequent thoracolumbar localization. These cases highlight the need for a detailed physical examination in diagnosing these commonly palpable tumors, which, though rare, should not be dismissed in patients with back pain. The cumulative evidence favors a surgical approach to management, emphasizing the need for knowledge and multi-disciplinary cooperation in diagnosing and treating this rare condition successfully.
Ethical Considerations
Compliance with ethical guidelines
This is a retrospective observational case study. The Ege University Research Ethics Committee has confirmed that no ethical approval is required. Consent to participate is not applicable as this is not an experimental study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Hüseyin Biçeroğlu, Mustafa Serdar Bölük, Taşkın Yurtseven; Data collection and drafting the article: Bilal Bahadır Akbulut and Mustafa Serdar Bölük; Data analysis and interpretation: Taner Akalın; Review, editing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Myxomas are mesenchymal tumors that are benign and are mainly found in cardiac tissues but are seldom ob-served in skeletal muscle tissues. Paraspinal intramuscular myxoma is even more of a rarity with limited studies that discuss clinical manifestations, diagnostic criteria, and treatment options [1–5]. Arising out of fibroblasts that are known to overproduce the mucinous extracellular matrix, these tumors are mostly of non-aggressive behavior but are a major diagnostic and therapeutic dilemma due to their anatomical location and the similari-ties in the presentation with other spindle cell neoplasms [6].
The rarity of paraspinal intramuscular myxomas and the critical anatomical relationship of the paraspinal region with the spinal structures only worsen the need for extensive research since the small number of documented cases does not allow for evidence-based clinical guidelines.
In this paper, we present an in-depth discussion of a case of intramuscular myxoma situated in the lumbar paraspinal musculature and a literature review of this rare entity.
2. Case Presentation
The case of this study was a 46-year-old female who presented with back pain exacerbating with movement over 3 months. A thoracolumbar magnetic resonance imaging (MRI) was performed (Figure 1), revealing a T2 hyperintense 35×25×85 mm mass that extends craniocaudally within the right-sided paraspinal muscles corresponding to the T11-L1 levels. There was heterogeneous contrast enhancement on T1 sequence images. Subsequent CT imaging revealed the lesion to be non-contrast enhancing and hypodense. Radiology suggested a myxoma or an abscess within the paraspinal musculature. Acute phase reactants were within normal levels, with CRP of 1 and WBC of 6.91. The mass within the paraspinal musculature can be visualized and palpated during the physical examination. The patient had no neurological symptoms.
The patient was operated under general anesthesia using a paramedian incision, paraspinal muscles were dissected and a rubbery mass was palpated within (Figure 2). The tumor was mobilized in all quadrants and removed with a 1 cm margin within the paraspinal muscles. The tumor had a gel-like internal substance. There was no complication intraoperatively and the wound was closed.
Histopathological examination revealed a tumor characterized by a loose arrangement of spindle-stellated cells on a distinct myxoid background. The tumor was surrounded by striated muscle tissue in large areas but was surrounded by a pseudocapsule in a focal area (Figure 3). No atypia or mitotic activity was observed in the cells (Figure 4). Immunohistological staining was focally positive for CD34 and smooth muscle actin but negative for desmin, S-100, MUC4, and SOX-10 protein. The tumor had a Ki67 of 1%.
The postoperative MRI scan revealed complete removal of the tumor and the patient was followed up for 2 days and discharged without complications.
3. Literature Review
Materials and Methods
A PubMed search was performed using “(intramuscular) AND (myxoma)” keywords in the PubMed-National Center for Biotechnology Information database. Two-hundred and sixty studies were found published before October 2023. Out of these, 18 papers were relevant, 14 of which were in English and had an available full-text (Figure 5).
4. Results
A total of 14 studies are included in this review, comprising 16 cases, including this case report (Table 1).
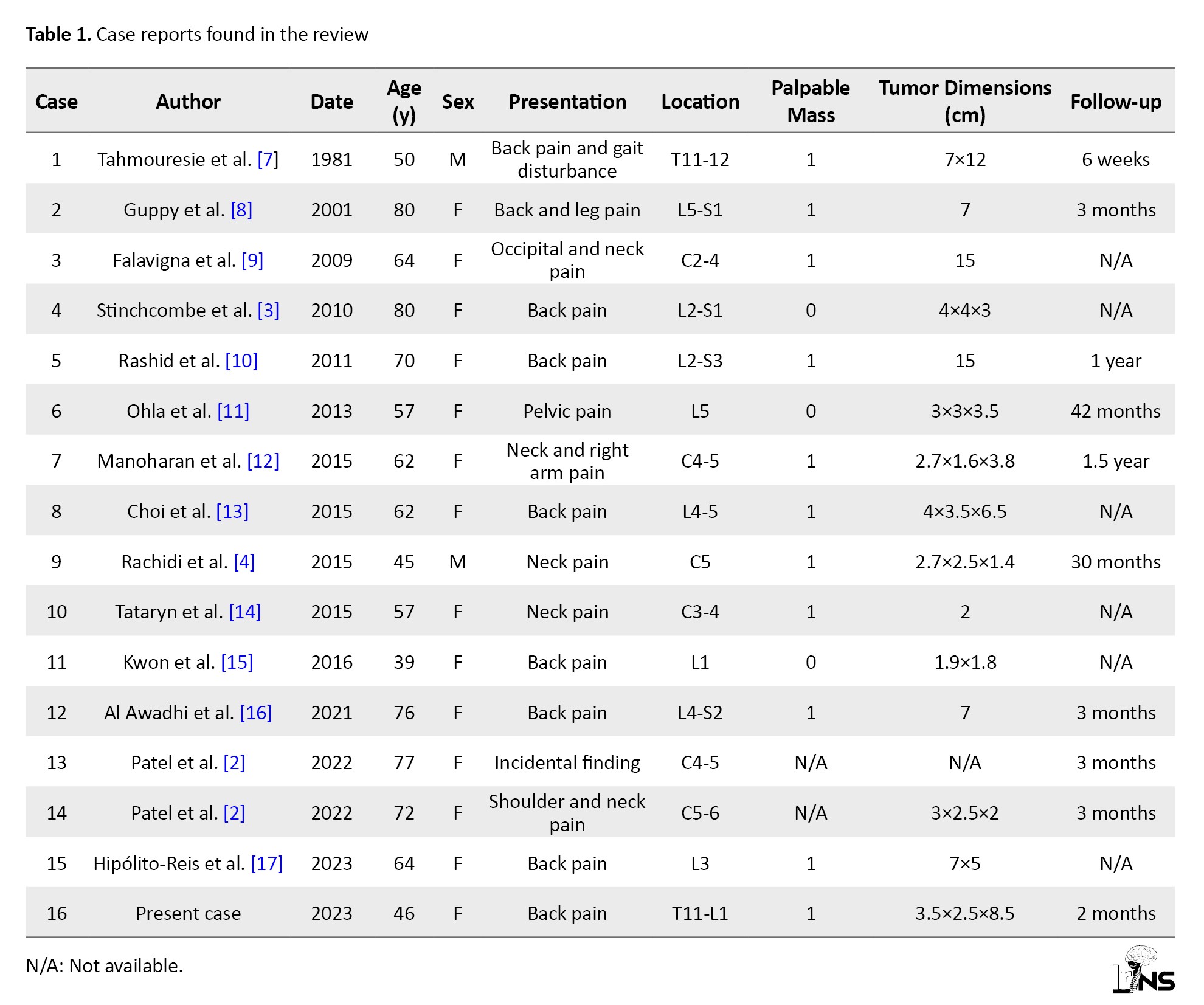
Median age was 63 (range 39-80), with female predominance (n=14, 87.5%). Most of the cases were located in the thoracolumbar area (n=10, 62.5%). Of the cases available, 78% had a palpable mass on presentation (n=11).
5. Discussion
Intramuscular myxomas are a rare paraspinal musculature pathology. As far as we know there have been 16 cases, including our present case.
This pathology most commonly presents as back pain, with radicular pain in cases of spinal canal involvement. Treatment paradigms are mainly centered on surgical resection for extramarginal resection with or without neurological function preservation as appropriate. The literature mirrors positive results with surgical treatment, in most cases with low rates of recurrence.
Back pain is a very common issue that has a 1-year incidence of any episode of low back pain ranging between 1.5% and 36% [18], which increases with age, up to the age of 60-65. In the literature, 78% (n=11) of the cases had a palpable mass on presentation, showing us how important it is to palpate the patient’s back and physically examine for any masses or signs that might explain the pain and might provide an early diagnosis.
The histopathological diagnosis of myxoma is mainly identified by myxoid stroma containing loose, stellate, or spindle-shaped cells with ill-defined outlines and a minimal amount of eosinophilic cytoplasm. The characteristic myxoid stroma is rich in hyaluronic acid and other mucopolysaccharides, giving the tumor a loose or gelatinous texture. The vascular pattern in myxomas often reveals poorly developed capillary-like vessels with sparse and thin walls. The cells’ nuclei are usually small, unremarkable, and lack significant pleomorphism or mitotic activity, a sign of a benign character. Immunohistochemical analysis is ancillary, vimentin is positive, and desmin and S100 protein are typically negative. The myxoid matrix is further enhanced by special staining procedures, especially Alcian blue which binds to mucopolysaccharides and helps distinguish the myxomas from other soft tissue tumors. The precise histological evaluation, combined with immunohistochemical staining, and probably molecular analyses, constitute the cornerstone for the definitive diagnosis of myxoma, differentiating it from other myxoid or spindle cell neoplasms in the differential diagnosis [19].
6. Conclusion
Myxomas in the paraspinal region are rare but important intramuscular tumors due to their propensity to mimic common back pain, requiring inclusion in the differential diagnoses. The total excision of the tumor, as was the case in this patient, led to symptom relief and a low risk of recurrence, highlighting surgery as the treatment of choice.
The accumulation of 16 documented cases, including this one, adds to the knowledge of paraspinal intramuscular myxomas with a female predominance and frequent thoracolumbar localization. These cases highlight the need for a detailed physical examination in diagnosing these commonly palpable tumors, which, though rare, should not be dismissed in patients with back pain. The cumulative evidence favors a surgical approach to management, emphasizing the need for knowledge and multi-disciplinary cooperation in diagnosing and treating this rare condition successfully.
Ethical Considerations
Compliance with ethical guidelines
This is a retrospective observational case study. The Ege University Research Ethics Committee has confirmed that no ethical approval is required. Consent to participate is not applicable as this is not an experimental study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Hüseyin Biçeroğlu, Mustafa Serdar Bölük, Taşkın Yurtseven; Data collection and drafting the article: Bilal Bahadır Akbulut and Mustafa Serdar Bölük; Data analysis and interpretation: Taner Akalın; Review, editing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Domino JS, Weindel S, Woodrow S. Multiple paraspinal intramuscular myxomas: Case report. Journal of Neurosurgery. 2019; 32(4):519-22. [DOI:10.3171/2019.9.SPINE19599] [PMID]
- Patel S, Suji T, Pang G, Alg VS, Visagan R, Reisz Z, et al. Spinal myxomas: Review of a rare entity. Journal of Surgical Case Reports. 2022; 2022(5):rjac221. [DOI:10.1093/jscr/rjac221] [PMID]
- Stinchcombe S, Kochhar R, Malkan D. Intramuscular myxoma of the paraspinal musculature. Journal of Medical Cases. 2010; 1(2):42-6. [DOI:10.4021/jmc37w]
- Rachidi S, Sood AJ, Rumboldt T, Day TA. Intramuscular myxoma of the paraspinal muscles: A case report and systematic review of the literature. Oncology Letters. 2016 ; 11(1):466-70. [DOI:10.3892/ol.2015.3864] [PMID]
- Hughes LP, Prodoehl JP, Elia CJ, Sabourin V, Curtis MT, Harrop JS. Intramuscular myxoma of the lumbar paraspinal musculature: Case report. SN Comprehensive Clinical Medicine. 2022; 4(1):123. [DOI:10.1007/s42399-022-01210-4]
- Zhang Y, Huang J, Ding J. Imaging manifestations and pathological analysis of intramuscular myxoma: A case report and literature review. Radiology Case Reports. 2020; 16(2):300-4. [DOI:10.1016/j.radcr.2020.10.053] [PMID]
- Tahmouresie A, Farmer PM, Stokes N. Paraspinal myxoma with spinal cord compression. Case report. Journal of Neurosurgery. 1981; 54(4):542-4. [DOI:10.3171/jns.1981.54.4.0542] [PMID]
- Guppy KH, Wagner F, Tawk R, Gallagher L. Intramuscular myxoma causing lumbar radiculopathy. Case report and review of the literature. Journal of Neurosurgery. 2001; 95(2 Suppl):260-3. [DOI:10.3171/spi.2001.95.2.0260] [PMID]
- Falavigna A, Righesso O, Volquind D, Teles AR. Intramuscular myxoma of the cervical paraspinal muscle. European Spine Journal. 2009; 18(Suppl 2):245-9. [DOI:10.1007/s00586-009-0933-9] [PMID]
- Rashid A, Abdul-Jabar HB, Karmani S, Rezajooi K, Casey AT. Giant paravertebral myxoma. European Spine Journal. 2011; 20(Suppl 2):S138-42. [DOI:10.1007/s00586-010-1442-6] [PMID]
- Ohla V, Ciarlini PDSC, Goldsmith JD, Kasper EM. Cellular myxoma of the lumbar spine. Surgical Neurology International. 2013; 4:82. [DOI:10.4103/2152-7806.113648] [PMID]
- Manoharan SR, Shaw AB, Arnold CA, Farhadi HF. Infiltrative intramuscular myxoma of the cervical spine: A case report. The Spine Journal. 2015; 15(1):e1-4. [DOI:10.1016/j.spinee.2014.09.008] [PMID]
- Choi DY, Kim JT, Kim J, Lee HJ. Atypical intramuscular myxoma of the lumbosacral paraspinal muscle: The first case report in Asian. Journal of Korean Neurosurgical Society. 2015; 58(6):566-70. [DOI:10.3340/jkns.2015.58.6.566] [PMID]
- Tataryn Z, Tracy J, Tsang C, Wu J, Heilman CB, Wein RO. Intramuscular myxoma of the cervical paraspinal musculature: Case report and review of the literature. American Journal of Otolaryngology. 2015; 36(2):273-6. [DOI:10.1016/j.amjoto.2014.10.010] [PMID]
- Kwon JY, Kim IS, Hong JT, Kim JY, Sung JH, Lee SW. Intramuscular myxoma of the lumbar paravertebral muscle. The Spine Journal. 2016; 16(7):e451-2. [DOI:10.1016/j.spinee.2016.01.011] [PMID]
- Al Awadhi A, Benichi S, Lot G, Rogers A. A case of intramuscular lumbar myxoma: Uncertainty in the preoperative diagnosis of a spinal soft tissue tumour. Neurochirurgie. 2022; 68(5):530-4. [DOI:10.1016/j.neuchi.2021.08.007] [PMID]
- Hipólito-Reis J, Roque D, Teixeira JC. Lumbar paraspinal intramuscular myxoma: A case report. Surgical Neurology International. 2023; 14:86. [DOI:10.25259/SNI_141_2023] [PMID]
- Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Practice & Research. Clinical Rheumatology. 2010; 24(6):769-81. [DOI:10.1016/j.berh.2010.10.002] [PMID]
- Wang JG, Li YJ, Liu H, Li NN, Zhao J, Xing XM. Clinicopathologic analysis of cardiac myxomas: Seven years’ experience with 61 patients. Journal of Thoracic Disease. 2012; 4(3):272-83. [PMID]
Type of Study: Case report |
Subject:
Spine
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |