Wed, Feb 4, 2026
Volume 10 - Continuous Publishing
Iran J Neurosurg 2024, 10 - Continuous Publishing: 38-48 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mehrpour S, Shafa S, Vatankhah M, Malekshoar M, Sanie Jahromi M S, Zarei T, et al . Pain Management Methods and Techniques in Lumbar Disc Surgery: A Narrative Review Study. Iran J Neurosurg 2024; 10 : 4
URL: http://irjns.org/article-1-396-en.html
URL: http://irjns.org/article-1-396-en.html
Somayeh Mehrpour1 

 , Shahram Shafa2
, Shahram Shafa2 

 , Majid Vatankhah3
, Majid Vatankhah3 

 , Mehrdad Malekshoar3
, Mehrdad Malekshoar3 

 , Mohammad Sadegh Sanie Jahromi3
, Mohammad Sadegh Sanie Jahromi3 

 , Tayyebeh Zarei4
, Tayyebeh Zarei4 

 , Mansour Deylami *5
, Mansour Deylami *5 

 , Fateme Maleki6
, Fateme Maleki6 

 , Roohie Farzaneh7
, Roohie Farzaneh7 




 , Shahram Shafa2
, Shahram Shafa2 

 , Majid Vatankhah3
, Majid Vatankhah3 

 , Mehrdad Malekshoar3
, Mehrdad Malekshoar3 

 , Mohammad Sadegh Sanie Jahromi3
, Mohammad Sadegh Sanie Jahromi3 

 , Tayyebeh Zarei4
, Tayyebeh Zarei4 

 , Mansour Deylami *5
, Mansour Deylami *5 

 , Fateme Maleki6
, Fateme Maleki6 

 , Roohie Farzaneh7
, Roohie Farzaneh7 


1- Department of Anesthesiology and Critical Care, School of Medicine, Qom University of Medical Sciences, Qom, Iran.
2- Department of Orthopedics, School of Medicine, Jahrom University of Medical Sciences, Jahrom, Iran.
3- Department of Anesthesiology, Anesthesiology and Critical Care and Pain Management Research Center, School of Medicine, Hormozgan University of Medical Sciences, Bandar Abbas, Iran.
4- Department of Anesthesiology, School of Medicine, Jahrom University of Medical Sciences, Jahrom, Iran.
5- Department of Anesthesiology and Critical Care, Faculty of Medicine, Golestan University of Medical Sciences, Gorgan, Iran. ,mansour.deylami@gmail.com
6- Department of Emergency Medicine, School of Medicine, Birjand University of Medical Sciences, Birjand, Iran.
7- Department of Emergency Medicine, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
2- Department of Orthopedics, School of Medicine, Jahrom University of Medical Sciences, Jahrom, Iran.
3- Department of Anesthesiology, Anesthesiology and Critical Care and Pain Management Research Center, School of Medicine, Hormozgan University of Medical Sciences, Bandar Abbas, Iran.
4- Department of Anesthesiology, School of Medicine, Jahrom University of Medical Sciences, Jahrom, Iran.
5- Department of Anesthesiology and Critical Care, Faculty of Medicine, Golestan University of Medical Sciences, Gorgan, Iran. ,
6- Department of Emergency Medicine, School of Medicine, Birjand University of Medical Sciences, Birjand, Iran.
7- Department of Emergency Medicine, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
Full Text [PDF 1007 kb]
(1321 Downloads)
| Abstract (HTML) (4356 Views)
Full Text: (2920 Views)
1. Introduction
Lumbar disc disorder (LDD) is a widespread and consequential pathology that exerts its influence on the intervertebral discs situated in the lumbar region of the spine [1]. Marked by persistent back pain and functional limitations, LDD underscores the importance of prompt intervention. Historical therapeutic modalities, such as intradermal injections (chemonucleolysis), were directed at de-innervating affected discs. In contrast, contemporary strategies encompass surgical interventions and conservative approaches, like physical therapy [2, 3]. Globally, the estimated incidence of lumbar degenerative spine disease is 3.63%, with Europe exhibiting the highest prevalence at 5.7% [4]. Symptomatic herniated lumbar discs demonstrate a prevalence ranging from 1 to 3%, a variation influenced by age and gender. Moreover, non-spinal low back pain, inclusive of LDDs, has a global prevalence that fluctuates between 30% and 80%, with an upward trend associated with advancing age [5]. Lumbar intervertebral disc herniations stand out as a primary reason for lumbar spine surgery in the working-age population, underscoring the imperative need to comprehend the epidemiology and pathophysiology of LDD for effective management and preventive strategies [6]. Critical in addressing lumbar disc herniation, lumbar disc surgeries play an important role in preventing the progression to chronic back pain and functional limitations if left untreated [7]. Procedures, such as discectomy involve the removal of herniated disc material to alleviate nerve pressure [8]. Personalized interventions are underscored by predictive factors for surgical outcomes, including sex and preoperative symptoms. The prevalence of lumbar disc herniation surgery exhibits variability, lacking a definitive correlation with preoperative patient characteristics [9]. Moreover, the estimated incidence of vascular complications post-lumbar disc surgery ranges from 1 to 5 per 10,000 disc operations [10]. Symptomatic lumbar spinal stenosis, a related condition, manifests in approximately 10% of patients aged over 65 years [11]. The criteria guiding the decision to perform surgery for treating symptomatic lumbar disc degeneration are not precisely defined, often relying on a case-by-case assessment dependent on specific clinical circumstances [12]. Lumbar disc pain is often associated with conditions such as lumbar disc herniation [13], which is important due to its potential to cause chronic back pain and functional limitations, thereby affecting daily activities and overall quality of life [13]. Addressing lumbar disc pain is necessary to prevent the exacerbation of symptoms, which may encompass pain, numbness, or weakness, significantly impeding daily activities [13].
Complications associated with lumbar disc issues, particularly herniated discs, may entail nerve injuries, dural puncture leading to positional headaches, infections, epidural abscess, epidural hematoma, paralysis, and the development of chronic back pain if left untreated [14]. Effective pain management is necessary for the success of disc disorder surgeries, influencing various aspects of the postoperative journey [15]. Swift recovery is facilitated as patients experience reduced discomfort, enabling an earlier return to normal activities. Beyond the immediate postoperative period, proficient pain control minimizes the risk of complications, such as infections and thrombosis, contributing to a smoother overall recovery process [16]. Patient comfort and satisfaction are heightened, fostering positive doctor-patient relationships and adherence to postoperative care instructions [17]. Implementing multimodal analgesia and non-opioid strategies not only lessens reliance on opioids and diminishes associated risks but also supports favorable long-term outcomes by encouraging early mobilization and participation in rehabilitation programs [18]. In essence, prioritizing pain management in surgeries for disc disorders is integral for optimizing patient outcomes, ensuring a positive surgical experience, and promoting long-term well-being [19]. The management of pain and provision of analgesia throughout all stages of surgery (preoperative, intraoperative and postoperative) is a critical procedure. This narrative review aimed to explore the many approaches and techniques of analgesia utilized in this context. It is employed in the field of spinal surgery.
2. Materials and Methods
Our search strategy involved employing a combination of pertinent keywords, such as ‘pain management,’ ‘lumbar disc surgery,’ ‘methods,’ AND ‘techniques.’ Using Boolean operators, we constructed a search query like (‘pain management’ OR ‘analgesia’) AND (‘lumbar disc surgery’ OR ‘spinal surgery’) AND (‘techniques’ OR ‘procedures’ OR ‘approaches’ OR ‘methods’) AND ‘narrative review.’ This approach included exploring reputable medical databases, like PubMed, MEDLINE, and Cochrane Library, with filters applied for publication type and date, focusing on articles published within the last 20 years. Additionally, the authors meticulously examined the search results, selecting the most relevant articles to ensure the inclusion of up-to-date and high-quality information in their review.
3. Results and Discussion
Opioid analgesics
Pain management after lumbar disc surgery often needs the administration of opioids [15]. Traditionally, opioids have been periodically supplied as necessary to manage postoperative pain after spinal surgery [20]. However, there is a growing interest in alternative strategies to reduce opioid use due to concerns about dependency and side effects [21, 22]. Studies have explored the efficacy of non-opioid analgesics, such as acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and COX-2 inhibitors, as a component of a multimodal strategy for pain management following intricate spinal surgery [17, 23]. The utilization of oxymorphone, nalbuphine, and buprenorphine has been examined in the context of pain management subsequent to lumbar disc surgery. It is noteworthy that preoperative sublingual administration of buprenorphine is recommended for its procedural simplicity and effectiveness in alleviating postoperative pain following lumbar disc surgery [24, 25]. Furthermore, the investigational use of intrathecal nalbuphine as an adjuvant in spinal anesthesia for orthopedic surgeries has been indicative of its efficacy in achieving pain relief [26, 27]. Sublingual buprenorphine has demonstrated effectiveness in the control of pain subsequent to procedures, such as lumbar laminectomy and discectomy [28]. Moreover, the proactive administration of intravenous nalbuphine before surgery has shown positive outcomes, particularly in affording visceral pain relief, a notable benefit for patients presenting with symptomatic gallbladder disease [29].
Low-dose intravenous ketamine
Low-dose intravenous ketamine has emerged as a valuable adjunct in pain management strategies following lumbar disc surgery. Perioperative administration of low-dose ketamine can provide effective analgesia, reduce opioid consumption, and contribute to a morphine-sparing effect without a significant increase in adverse events after spine surgery [30-32]. This approach is very advantageous in reducing opioid demands in patients with chronic back pain undergoing surgery, thereby improving pain control and reducing the risk of opioid-related complications [33, 34]. Moreover, the amalgamation of low-dose ketamine with lidocaine as an adjunctive component augments the efficacy of low-dose ketamine in the management of pain following lumbar disc surgeries [35]. Some studies have been conducted on the effectiveness of low-dose ketamine as a pain management solution. These studies have consistently shown that ketamine can reduce intraoperative pain and provide short-term pain relief for up to 24 hours after surgery. However, it is worth noting that this pain reduction is not sustained over a longer period [35-37].
Epidural analgesia
Epidural analgesia is a notable pain management technique employed in lumbar disc surgery [38]. Studies have shown its effectiveness in providing postoperative pain relief and reducing the need for systemic analgesia [39, 40]. Intraoperative epidural analgesia, whether with nonsteroidal agents or other medications, has demonstrated efficacy in diminishing postoperative pain and analgesic consumption [41]. This technique is particularly valuable in severe spinal surgical interventions, aiding in managing the complexity and intensity of pain associated with lumbar disc surgery [42, 43].
Epidural administration of steroids
Epidural administration of steroids is a valuable approach in pain management for lumbar disc surgery. Studies have demonstrated that perioperative steroids contribute to better control of both back and leg pain post-surgery, leading to improved patient outcomes [44, 45]. Some surgeons have utilized the administration of epidural corticosteroids and local anesthetics during surgery for a herniated lumbar disc in order to alleviate postoperative discomfort [46]. Additionally, lumbar epidural steroid injections have been utilized to alleviate low back pain and sciatica, providing targeted relief in the affected area [47]. The effectiveness of intra-venous steroids as part of conservative treatment options, including oral and parenteral delivery, has also been explored to prevent complications and enhance recovery [48]. Overall, epidural administration of steroids proves to be a valuable component in multimodal pain management strategies for lumbar disc surgery. It seems that there is no clear agreement among studies on the effectiveness of using this method for chronic back pain management [48, 49].
According to Lee et al. (2018), both steroids and local anesthetics can effectively manage pain in disc surgery patients. However, when it comes to long-term pain control, they suggest that steroids might be a stronger option. The reason behind this is that the individuals who received steroids showed considerable improvement in pain control at 1, 3 and 6 months post-surgery [49]. In contrast, Samoladas et al. showed that intraoperative use of steroids and local anesthetic was effective in reducing pain only for a short time after surgery, while compared to the placebo, it did not affect the rate of infection or other long-term consequences [50].
Local anesthetic wound infiltration and catheter placement
Local anesthetic wound infiltration and catheter placement are commonly utilized methods in postoperative pain management. Wound infiltration involves the use of local anesthetics directly at the surgical area, proving to be an increasingly common technique for controlling postoperative pain [51-53]. This approach is particularly effective in minor surgeries, such as laceration repairs and skin procedures [54, 55]. Catheter placement involves the insertion of a catheter, often epidural or local anesthesia, for continuous administration of analgesics, providing sustained pain relief. In spine surgeries, options, like local anesthetic wound infiltration or catheter placement, along with spinal and epidural anesthesia, are considered for appropriate perioperative pain management [16]. In conclusion, both techniques aim to enhance patient comfort and reduce the need for systemic opioids, contributing to improved recovery outcomes.
NSAIDs
NSAIDs have been found to be effective in the perioperative and postoperative pain management of lumbar disc surgery. The incorporation of NSAIDs with opioid analgesics provides better pain control after lumbar spine surgery, resulting in significantly improved pain scores compared to a placebo [16, 56-58]. A meta-analysis of randomized controlled trials further supports the effectiveness of NSAIDs in postoperative pain management after lumbar spine surgery [59].
Acetaminophen
Acetaminophen has a role in postoperative pain control following lumbar disc surgery. While over-the-counter acetaminophen can be used to alleviate pain, evidence for its effectiveness as the sole agent for preventing postsurgical pain after spinal surgery is limited [60]. Some studies have suggested that intravenous acetaminophen IV effectively reduces postoperative pain and overall analgesic dosage after certain surgeries, such as craniotomy, but its impact on lumbar disc surgery may vary [15, 17]. Additionally, a study on minimally invasive spine surgery found no significant effect on postoperative pain with perioperative intravenous acetaminophen. The pain relief treatment for complicated spine surgery often involves administering acetaminophen before or during the surgery, along with COX-2 specific inhibitors or NSAIDs for ongoing pain control [61].
Peripheral nerve blocks
Peripheral nerve blocks have proven effective in managing pain associated with lumbar disc surgery. These blocks can be used to alleviate chronic lumbosacral radiculopathy, providing relief for patients dealing with persistent pain [62]. Furthermore, peripheral nerve blocks play a significant role in pain management for various surgical procedures, including lumbar disc surgery [63]. By blocking certain nerves, these blocks provide tailored pain relief when injected close to the nerves that govern sensation [64]. When dealing with either acute or chronic back pain, peripheral nerve blocks are thought to be a useful method [65].
Gabapentin and pregabalin
Gabapentin and pregabalin have demonstrated effectiveness in managing pain after lumbar disc surgery. Both medications are effective by reducing postoperative discomfort, minimizing the need for narcotics, and offering respite to patients undergoing spine surgery [66, 67]. Analgesic effects of gabapentin and pregabalin have been demonstrated in the management of pain caused by neuropathic pain, contributing to their use in postoperative pain management. Studies have investigated different dosages of these medications, providing evidence for their effectiveness in pain relief after spinal surgery [67, 68].
Postoperative physical therapy and rehabilitation
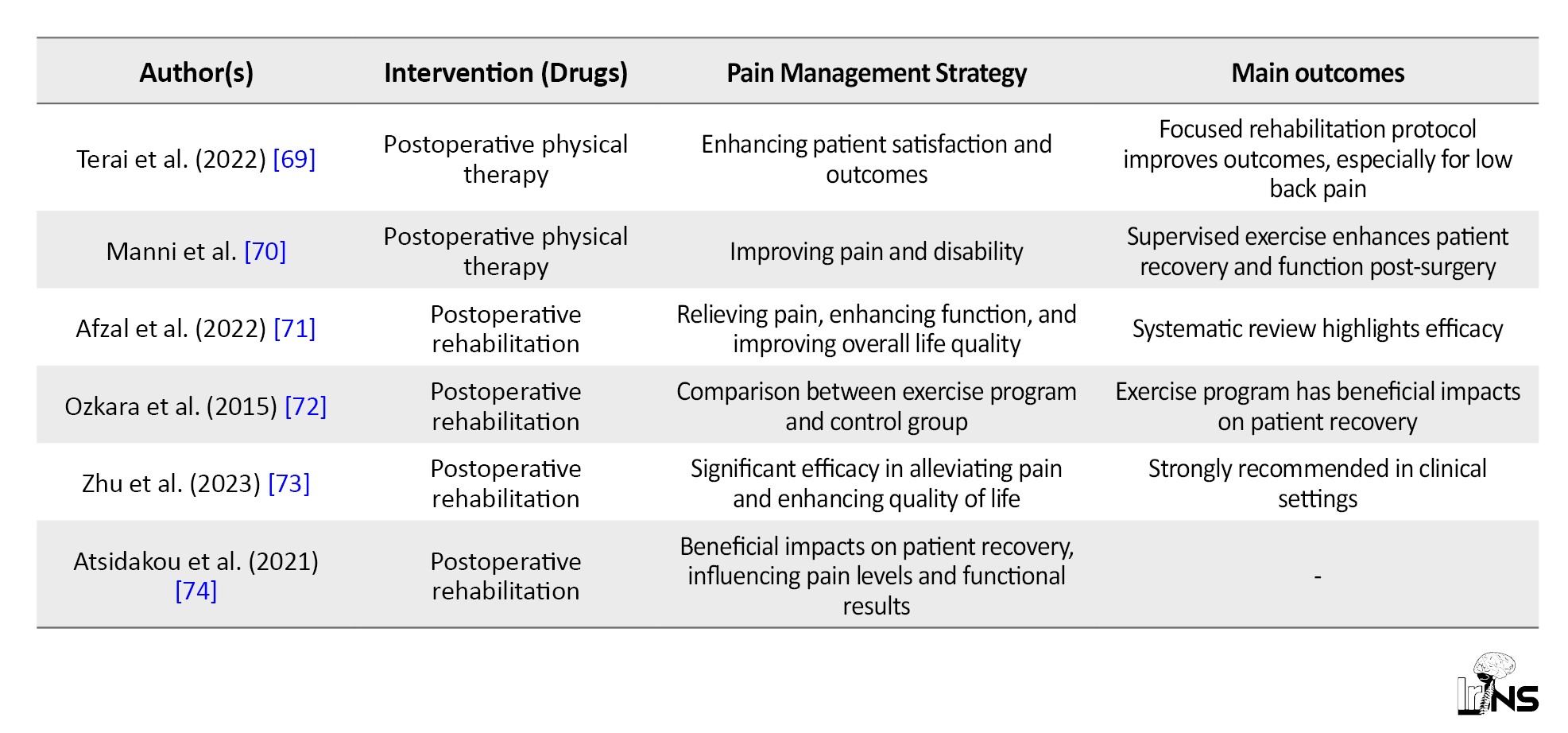
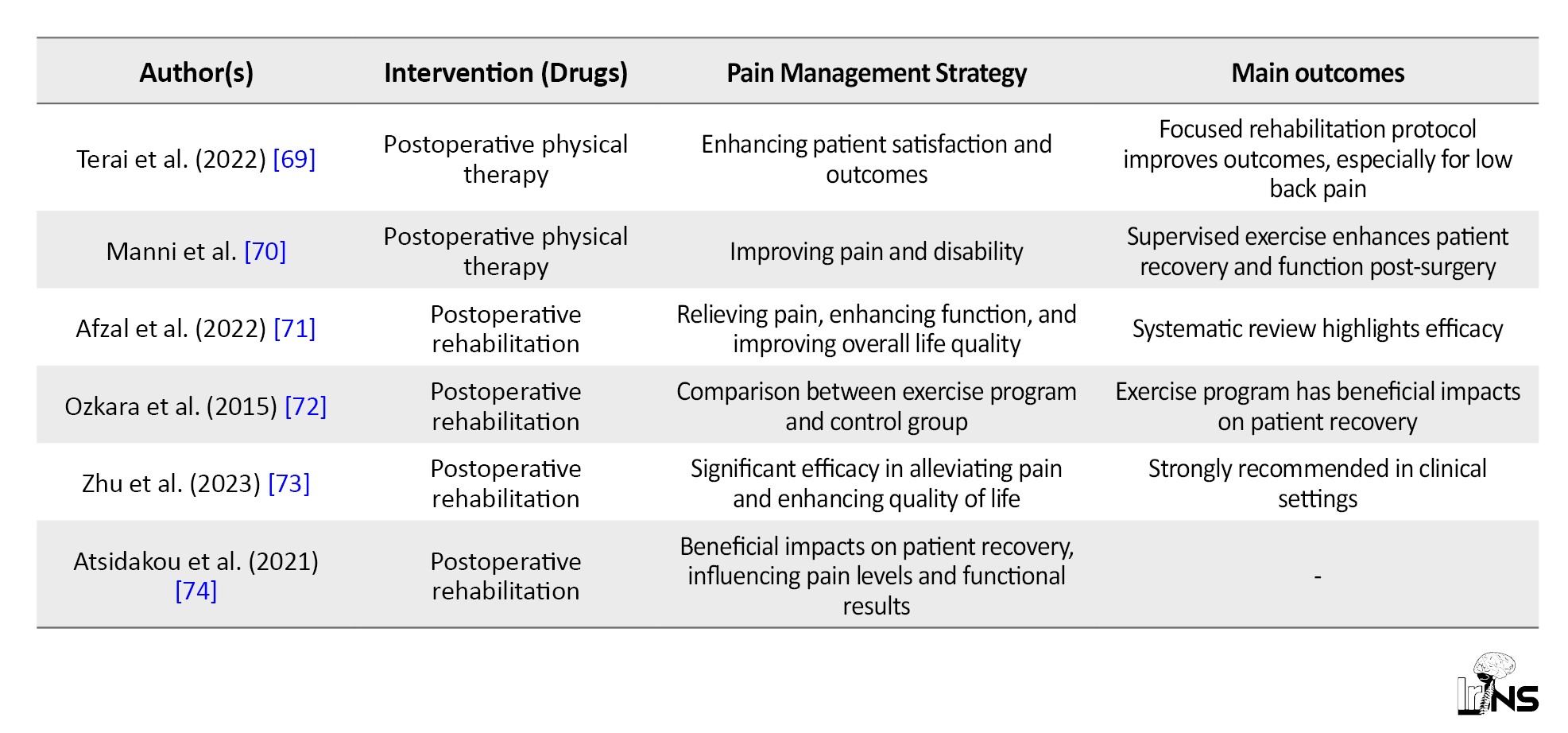
Postoperative physical therapy is essential for effectively managing pain after lumbar disc surgery. A focused rehabilitation protocol following surgery, especially one targeting low back pain, enhances patient satisfaction with therapy following minimally invasive lumbar decompression operations [69]. The effectiveness of postoperative physical therapy extends to improving patient outcomes, including pain and disability, after lumbar surgery. Supervised exercise, as part of a rehabilitation program, has shown promise in enhancing patient recovery and function post-surgery [16, 70].
Postoperative rehabilitation following lumbar disc surgery is an essential component of patient treatment, with a primary focus on enhancing patient outcomes and effectively managing pain. A systematic review highlighted the efficacy of postoperative rehabilitation in relieving pain, enhancing function, and improving the overall life quality of individuals with lumbar disc surgery [71]. A randomized investigation made a comparison between an exercise program and a control group in terms of pain, back impairment, and behavioral outcomes following lumbar disc surgery. The study revealed that the exercise program had beneficial impacts on patient recovery [72]. Postoperative rehabilitation training has demonstrated significant efficacy in alleviating pain and enhancing quality of life, making it strongly recommended in clinical settings [73]. The implementation of active physiotherapeutic rehabilitation following lumbar disc surgery has shown beneficial impacts on patient recovery, influencing both pain levels and functional results [74] (Table 1).


4. Conclusion
Opioids, while demonstrating efficacy, pose difficulties that necessitate contemplation of alternate options. Low-dose ketamine, epidural analgesia, and steroid epidurals are emerging as effective strategies, each with distinct advantages in alleviating postoperative pain and enhancing outcomes. Postoperative pain control after lumbar disc surgery involves the administration of local anesthetic to the surgical area, the insertion of a catheter for continuous pain relief, and the utilization of NSAIDs, acetaminophen, and external nerve blocks. The use of gabapentin/pregabalin, in conjunction with physical therapy, effectively alleviates pain and enhances functionality following surgical procedures. Implementing these measures thoroughly enhances patient comfort and improves the overall quality of life following lumbar disc surgery. One of the notable aspects of this study is its thorough examination of different pharmacological treatments used in surgical procedures and pain management. By integrating viewpoints from both opioid and non-opioid perspectives, this method addresses current concerns around opioid dependency and side effects and offers a well-rounded and detailed plan. This narrative review of lumbar disc surgery pain management has certain limitations. The inclusion of studies with diverse methodologies introduces potential variability in the quality of evidence. The heterogeneity in surgical procedures and patient populations limits generalizability. It is suggested that future quantitative studies and meta-analyses investigate pain control techniques and drugs in different phases before, during and after surgery.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally in performing the project and preparing the manuscript.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgements
The authors would like to thank the Clinical Research Development Unit of Peymanieh Educational and Research and Therapeutic Center of Jahrom University of Medical Sciences for providing facilities for this work.
References
Lumbar disc disorder (LDD) is a widespread and consequential pathology that exerts its influence on the intervertebral discs situated in the lumbar region of the spine [1]. Marked by persistent back pain and functional limitations, LDD underscores the importance of prompt intervention. Historical therapeutic modalities, such as intradermal injections (chemonucleolysis), were directed at de-innervating affected discs. In contrast, contemporary strategies encompass surgical interventions and conservative approaches, like physical therapy [2, 3]. Globally, the estimated incidence of lumbar degenerative spine disease is 3.63%, with Europe exhibiting the highest prevalence at 5.7% [4]. Symptomatic herniated lumbar discs demonstrate a prevalence ranging from 1 to 3%, a variation influenced by age and gender. Moreover, non-spinal low back pain, inclusive of LDDs, has a global prevalence that fluctuates between 30% and 80%, with an upward trend associated with advancing age [5]. Lumbar intervertebral disc herniations stand out as a primary reason for lumbar spine surgery in the working-age population, underscoring the imperative need to comprehend the epidemiology and pathophysiology of LDD for effective management and preventive strategies [6]. Critical in addressing lumbar disc herniation, lumbar disc surgeries play an important role in preventing the progression to chronic back pain and functional limitations if left untreated [7]. Procedures, such as discectomy involve the removal of herniated disc material to alleviate nerve pressure [8]. Personalized interventions are underscored by predictive factors for surgical outcomes, including sex and preoperative symptoms. The prevalence of lumbar disc herniation surgery exhibits variability, lacking a definitive correlation with preoperative patient characteristics [9]. Moreover, the estimated incidence of vascular complications post-lumbar disc surgery ranges from 1 to 5 per 10,000 disc operations [10]. Symptomatic lumbar spinal stenosis, a related condition, manifests in approximately 10% of patients aged over 65 years [11]. The criteria guiding the decision to perform surgery for treating symptomatic lumbar disc degeneration are not precisely defined, often relying on a case-by-case assessment dependent on specific clinical circumstances [12]. Lumbar disc pain is often associated with conditions such as lumbar disc herniation [13], which is important due to its potential to cause chronic back pain and functional limitations, thereby affecting daily activities and overall quality of life [13]. Addressing lumbar disc pain is necessary to prevent the exacerbation of symptoms, which may encompass pain, numbness, or weakness, significantly impeding daily activities [13].
Complications associated with lumbar disc issues, particularly herniated discs, may entail nerve injuries, dural puncture leading to positional headaches, infections, epidural abscess, epidural hematoma, paralysis, and the development of chronic back pain if left untreated [14]. Effective pain management is necessary for the success of disc disorder surgeries, influencing various aspects of the postoperative journey [15]. Swift recovery is facilitated as patients experience reduced discomfort, enabling an earlier return to normal activities. Beyond the immediate postoperative period, proficient pain control minimizes the risk of complications, such as infections and thrombosis, contributing to a smoother overall recovery process [16]. Patient comfort and satisfaction are heightened, fostering positive doctor-patient relationships and adherence to postoperative care instructions [17]. Implementing multimodal analgesia and non-opioid strategies not only lessens reliance on opioids and diminishes associated risks but also supports favorable long-term outcomes by encouraging early mobilization and participation in rehabilitation programs [18]. In essence, prioritizing pain management in surgeries for disc disorders is integral for optimizing patient outcomes, ensuring a positive surgical experience, and promoting long-term well-being [19]. The management of pain and provision of analgesia throughout all stages of surgery (preoperative, intraoperative and postoperative) is a critical procedure. This narrative review aimed to explore the many approaches and techniques of analgesia utilized in this context. It is employed in the field of spinal surgery.
2. Materials and Methods
Our search strategy involved employing a combination of pertinent keywords, such as ‘pain management,’ ‘lumbar disc surgery,’ ‘methods,’ AND ‘techniques.’ Using Boolean operators, we constructed a search query like (‘pain management’ OR ‘analgesia’) AND (‘lumbar disc surgery’ OR ‘spinal surgery’) AND (‘techniques’ OR ‘procedures’ OR ‘approaches’ OR ‘methods’) AND ‘narrative review.’ This approach included exploring reputable medical databases, like PubMed, MEDLINE, and Cochrane Library, with filters applied for publication type and date, focusing on articles published within the last 20 years. Additionally, the authors meticulously examined the search results, selecting the most relevant articles to ensure the inclusion of up-to-date and high-quality information in their review.
3. Results and Discussion
Opioid analgesics
Pain management after lumbar disc surgery often needs the administration of opioids [15]. Traditionally, opioids have been periodically supplied as necessary to manage postoperative pain after spinal surgery [20]. However, there is a growing interest in alternative strategies to reduce opioid use due to concerns about dependency and side effects [21, 22]. Studies have explored the efficacy of non-opioid analgesics, such as acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and COX-2 inhibitors, as a component of a multimodal strategy for pain management following intricate spinal surgery [17, 23]. The utilization of oxymorphone, nalbuphine, and buprenorphine has been examined in the context of pain management subsequent to lumbar disc surgery. It is noteworthy that preoperative sublingual administration of buprenorphine is recommended for its procedural simplicity and effectiveness in alleviating postoperative pain following lumbar disc surgery [24, 25]. Furthermore, the investigational use of intrathecal nalbuphine as an adjuvant in spinal anesthesia for orthopedic surgeries has been indicative of its efficacy in achieving pain relief [26, 27]. Sublingual buprenorphine has demonstrated effectiveness in the control of pain subsequent to procedures, such as lumbar laminectomy and discectomy [28]. Moreover, the proactive administration of intravenous nalbuphine before surgery has shown positive outcomes, particularly in affording visceral pain relief, a notable benefit for patients presenting with symptomatic gallbladder disease [29].
Low-dose intravenous ketamine
Low-dose intravenous ketamine has emerged as a valuable adjunct in pain management strategies following lumbar disc surgery. Perioperative administration of low-dose ketamine can provide effective analgesia, reduce opioid consumption, and contribute to a morphine-sparing effect without a significant increase in adverse events after spine surgery [30-32]. This approach is very advantageous in reducing opioid demands in patients with chronic back pain undergoing surgery, thereby improving pain control and reducing the risk of opioid-related complications [33, 34]. Moreover, the amalgamation of low-dose ketamine with lidocaine as an adjunctive component augments the efficacy of low-dose ketamine in the management of pain following lumbar disc surgeries [35]. Some studies have been conducted on the effectiveness of low-dose ketamine as a pain management solution. These studies have consistently shown that ketamine can reduce intraoperative pain and provide short-term pain relief for up to 24 hours after surgery. However, it is worth noting that this pain reduction is not sustained over a longer period [35-37].
Epidural analgesia
Epidural analgesia is a notable pain management technique employed in lumbar disc surgery [38]. Studies have shown its effectiveness in providing postoperative pain relief and reducing the need for systemic analgesia [39, 40]. Intraoperative epidural analgesia, whether with nonsteroidal agents or other medications, has demonstrated efficacy in diminishing postoperative pain and analgesic consumption [41]. This technique is particularly valuable in severe spinal surgical interventions, aiding in managing the complexity and intensity of pain associated with lumbar disc surgery [42, 43].
Epidural administration of steroids
Epidural administration of steroids is a valuable approach in pain management for lumbar disc surgery. Studies have demonstrated that perioperative steroids contribute to better control of both back and leg pain post-surgery, leading to improved patient outcomes [44, 45]. Some surgeons have utilized the administration of epidural corticosteroids and local anesthetics during surgery for a herniated lumbar disc in order to alleviate postoperative discomfort [46]. Additionally, lumbar epidural steroid injections have been utilized to alleviate low back pain and sciatica, providing targeted relief in the affected area [47]. The effectiveness of intra-venous steroids as part of conservative treatment options, including oral and parenteral delivery, has also been explored to prevent complications and enhance recovery [48]. Overall, epidural administration of steroids proves to be a valuable component in multimodal pain management strategies for lumbar disc surgery. It seems that there is no clear agreement among studies on the effectiveness of using this method for chronic back pain management [48, 49].
According to Lee et al. (2018), both steroids and local anesthetics can effectively manage pain in disc surgery patients. However, when it comes to long-term pain control, they suggest that steroids might be a stronger option. The reason behind this is that the individuals who received steroids showed considerable improvement in pain control at 1, 3 and 6 months post-surgery [49]. In contrast, Samoladas et al. showed that intraoperative use of steroids and local anesthetic was effective in reducing pain only for a short time after surgery, while compared to the placebo, it did not affect the rate of infection or other long-term consequences [50].
Local anesthetic wound infiltration and catheter placement
Local anesthetic wound infiltration and catheter placement are commonly utilized methods in postoperative pain management. Wound infiltration involves the use of local anesthetics directly at the surgical area, proving to be an increasingly common technique for controlling postoperative pain [51-53]. This approach is particularly effective in minor surgeries, such as laceration repairs and skin procedures [54, 55]. Catheter placement involves the insertion of a catheter, often epidural or local anesthesia, for continuous administration of analgesics, providing sustained pain relief. In spine surgeries, options, like local anesthetic wound infiltration or catheter placement, along with spinal and epidural anesthesia, are considered for appropriate perioperative pain management [16]. In conclusion, both techniques aim to enhance patient comfort and reduce the need for systemic opioids, contributing to improved recovery outcomes.
NSAIDs
NSAIDs have been found to be effective in the perioperative and postoperative pain management of lumbar disc surgery. The incorporation of NSAIDs with opioid analgesics provides better pain control after lumbar spine surgery, resulting in significantly improved pain scores compared to a placebo [16, 56-58]. A meta-analysis of randomized controlled trials further supports the effectiveness of NSAIDs in postoperative pain management after lumbar spine surgery [59].
Acetaminophen
Acetaminophen has a role in postoperative pain control following lumbar disc surgery. While over-the-counter acetaminophen can be used to alleviate pain, evidence for its effectiveness as the sole agent for preventing postsurgical pain after spinal surgery is limited [60]. Some studies have suggested that intravenous acetaminophen IV effectively reduces postoperative pain and overall analgesic dosage after certain surgeries, such as craniotomy, but its impact on lumbar disc surgery may vary [15, 17]. Additionally, a study on minimally invasive spine surgery found no significant effect on postoperative pain with perioperative intravenous acetaminophen. The pain relief treatment for complicated spine surgery often involves administering acetaminophen before or during the surgery, along with COX-2 specific inhibitors or NSAIDs for ongoing pain control [61].
Peripheral nerve blocks
Peripheral nerve blocks have proven effective in managing pain associated with lumbar disc surgery. These blocks can be used to alleviate chronic lumbosacral radiculopathy, providing relief for patients dealing with persistent pain [62]. Furthermore, peripheral nerve blocks play a significant role in pain management for various surgical procedures, including lumbar disc surgery [63]. By blocking certain nerves, these blocks provide tailored pain relief when injected close to the nerves that govern sensation [64]. When dealing with either acute or chronic back pain, peripheral nerve blocks are thought to be a useful method [65].
Gabapentin and pregabalin
Gabapentin and pregabalin have demonstrated effectiveness in managing pain after lumbar disc surgery. Both medications are effective by reducing postoperative discomfort, minimizing the need for narcotics, and offering respite to patients undergoing spine surgery [66, 67]. Analgesic effects of gabapentin and pregabalin have been demonstrated in the management of pain caused by neuropathic pain, contributing to their use in postoperative pain management. Studies have investigated different dosages of these medications, providing evidence for their effectiveness in pain relief after spinal surgery [67, 68].
Postoperative physical therapy and rehabilitation
Postoperative physical therapy is essential for effectively managing pain after lumbar disc surgery. A focused rehabilitation protocol following surgery, especially one targeting low back pain, enhances patient satisfaction with therapy following minimally invasive lumbar decompression operations [69]. The effectiveness of postoperative physical therapy extends to improving patient outcomes, including pain and disability, after lumbar surgery. Supervised exercise, as part of a rehabilitation program, has shown promise in enhancing patient recovery and function post-surgery [16, 70].
Postoperative rehabilitation following lumbar disc surgery is an essential component of patient treatment, with a primary focus on enhancing patient outcomes and effectively managing pain. A systematic review highlighted the efficacy of postoperative rehabilitation in relieving pain, enhancing function, and improving the overall life quality of individuals with lumbar disc surgery [71]. A randomized investigation made a comparison between an exercise program and a control group in terms of pain, back impairment, and behavioral outcomes following lumbar disc surgery. The study revealed that the exercise program had beneficial impacts on patient recovery [72]. Postoperative rehabilitation training has demonstrated significant efficacy in alleviating pain and enhancing quality of life, making it strongly recommended in clinical settings [73]. The implementation of active physiotherapeutic rehabilitation following lumbar disc surgery has shown beneficial impacts on patient recovery, influencing both pain levels and functional results [74] (Table 1).


4. Conclusion
Opioids, while demonstrating efficacy, pose difficulties that necessitate contemplation of alternate options. Low-dose ketamine, epidural analgesia, and steroid epidurals are emerging as effective strategies, each with distinct advantages in alleviating postoperative pain and enhancing outcomes. Postoperative pain control after lumbar disc surgery involves the administration of local anesthetic to the surgical area, the insertion of a catheter for continuous pain relief, and the utilization of NSAIDs, acetaminophen, and external nerve blocks. The use of gabapentin/pregabalin, in conjunction with physical therapy, effectively alleviates pain and enhances functionality following surgical procedures. Implementing these measures thoroughly enhances patient comfort and improves the overall quality of life following lumbar disc surgery. One of the notable aspects of this study is its thorough examination of different pharmacological treatments used in surgical procedures and pain management. By integrating viewpoints from both opioid and non-opioid perspectives, this method addresses current concerns around opioid dependency and side effects and offers a well-rounded and detailed plan. This narrative review of lumbar disc surgery pain management has certain limitations. The inclusion of studies with diverse methodologies introduces potential variability in the quality of evidence. The heterogeneity in surgical procedures and patient populations limits generalizability. It is suggested that future quantitative studies and meta-analyses investigate pain control techniques and drugs in different phases before, during and after surgery.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally in performing the project and preparing the manuscript.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgements
The authors would like to thank the Clinical Research Development Unit of Peymanieh Educational and Research and Therapeutic Center of Jahrom University of Medical Sciences for providing facilities for this work.
References
- Donnally III CJ, Hanna A, Varacallo M. Lumbar degenerative disk disease. Treasure Island: StatPearls; 2023. [Link]
- Kos N, Gradisnik L, Velnar T. A brief review of the degenerative intervertebral disc disease. Medical Archives. 2019; 73(6):421-4. [DOI:10.5455/medarh.2019.73.421-424] [PMID] [PMCID]
- Amin RM, Andrade NS, Neuman BJ. Lumbar disc herniation. Current Reviews in Musculoskeletal Medicine. 2017; 10(4):507-16. [DOI:10.1007/s12178-017-9441-4] [PMID] [PMCID]
- Ravindra VM, Senglaub SS, Rattani A, Dewan MC, Härtl R, Bisson E, et al. Degenerative lumbar spine disease: Estimating global incidence and worldwide volume. Global Spine Journal. 2018; 8(8):784-94. [DOI:10.1177/2192568218770769] [PMID] [PMCID]
- Shokri P, Zahmatyar M, Falah Tafti M, Fathy M, Rezaei Tolzali M, Ghaffari Jolfayi A, et al. Non-spinal low back pain: Global epidemiology, trends, and risk factors. Health Science Reports. 2023; 6(9):e1533. [DOI:10.1002/hsr2.1533] [PMID] [PMCID]
- Schroeder GD, Guyre CA, Vaccaro AR. The epidemiology and pathophysiology of lumbar disc herniations. Seminars in Spine Surgery. 2016; 28(1):2-7. [DOI:10.1053/j.semss.2015.08.003]
- Sedighi M, Haghnegahdar A. Lumbar disk herniation surgery: Outcome and predictors. Global Spine Journal. 2014; 4(4):233-44. [DOI:10.1055/s-0034-1390010] [PMID] [PMCID]
- Donnally CJ 3rd, Madhavan K, Butler AJ, Sheu JI, Massel DH, Green BA, et al. A novel technique for stabilization of high-grade spondylolisthesis with transvertebral fusion without reduction. Journal of Clinical Neuroscience. 2019; 60:170-5. [DOI:10.1016/j.jocn.2018.11.001] [PMID]
- Lagerbäck T, Fritzell P, Hägg O, Nordvall D, Lønne G, Solberg TK, et al. Effectiveness of surgery for sciatica with disc herniation is not substantially affected by differences in surgical incidences among three countries: Results from the Danish, Swedish and Norwegian spine registries. European Spine Journal . 2019; 28(11):2562-71. [DOI:10.1007/s00586-018-5768-9] [PMID]
- Wilson CA, Roffey DM, Chow D, Alkherayf F, Wai EK. A systematic review of preoperative predictors for postoperative clinical outcomes following lumbar discectomy. The Spine Journal. 2016; 16(11):1413-22. [DOI:10.1016/j.spinee.2016.08.003] [PMID]
- Wu AM, Zou F, Cao Y, Xia DD, He W, Zhu B, et al. Lumbar spinal stenosis: An update on the epidemiology, diagnosis and treatment. AME Medical Journal. 2017; 2(5):1-15. [DOI:10.21037/amj.2017.04.13]
- Kim CH, Chung CK, Choi Y, Kim MJ, Yim D, Yang SH, et al. The long-term reoperation rate following surgery for lumbar herniated intervertebral disc disease: A nationwide sample cohort study with a 10-year follow-up. Spine. 2019; 44(19):1382-9. [DOI:10.1097/BRS.0000000000003065] [PMID]
- Buenaventura RM, Shah RV, Patel V, Benyamin R, Singh V. Systematic review of discography as a diagnostic test for spinal pain: An update. Pain Physician. 2007; 10(1):147. [DOI:10.36076/ppj.2007/10/147] [PMID]
- Urits I, Viswanath O, Galasso AC, Sottosani ER, Mahan KM, Aiudi CM, et al. Platelet-rich plasma for the treatment of low back pain: A comprehensive review. Current Pain and Headache Reports. 2019; 23(7):52. [DOI:10.1007/s11916-019-0757-1] [PMID]
- Bajwa SJ, Haldar R. Pain management following spinal surgeries: An appraisal of the available options. Journal of Craniovertebral Junction & Spine. 2015; 6(3):105-10. [DOI:10.4103/0974-8237.161589] [PMID] [PMCID]
- Prabhakar NK, Chadwick AL, Nwaneshiudu C, Aggarwal A, Salmasi V, Lii TR, et al. Management of postoperative pain in patients following spine surgery: A narrative review. International Journal of General Medicine. 2022; 15:4535-49. [DOI:10.2147/IJGM.S292698] [PMID] [PMCID]
- Waelkens P, Alsabbagh E, Sauter A, Joshi GP, Beloeil H; PROSPECT Working group of the European Society of Regional Anaesthesia and Pain therapy. Pain management after complex spine surgery: A systematic review and procedure-specific postoperative pain management recommendations. European Journal of Anaesthesiology. 2021; 38(9):985-94. [DOI:10.1097/EJA.0000000000001448] [PMID] [PMCID]
- Small C, Laycock H. Acute postoperative pain management. The British Journal of Surgery. 2020; 107(2):e70-80. [DOI:10.1002/bjs.11477] [PMID]
- Yoo JS, Ahn J, Buvanendran A, Singh K. Multimodal analgesia in pain management after spine surgery. Journal of Spine Surgery. 2019; 5(Suppl 2):S154-9. [DOI:10.21037/jss.2019.05.04] [PMID] [PMCID]
- Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC clinical practice guideline for prescribing opioids for pain - United States, 2022. MMWR. Recommendations and Reports. 2022; 71(3):1-95. [DOI:10.15585/mmwr.rr7103a1] [PMID] [PMCID]
- Patel AA, Walker CT, Prendergast V, Radosevich JJ, Grimm D, Godzik J, et al. Patient-controlled analgesia following lumbar spinal fusion surgery is associated with increased opioid consumption and opioid-related adverse events. Neurosurgery. 2020; 87(3):592-601. [DOI:10.1093/neuros/nyaa111] [PMID]
- Wright AK, Sikora M, Leveque JC. Characterizing the risk of long-term opioid utilization in patients undergoing lumbar spine surgery. Spine. 2020; 45(1):E54-60. [DOI:10.1097/BRS.0000000000003199] [PMID]
- Reed LA, Patel M, Luque K, Theiss SM. Opioid sparing analgesics in spine surgery. Advances in Orthopedics. 2022; 2022:1026547. [DOI:10.1155/2022/1026547] [PMID] [PMCID]
- Kiabi FH, Emadi SA, Shafizad M, Jelodar AG, Deylami H. The effect of preoperative sublingual buprenorphine on postoperative pain after lumbar discectomy: A randomized controlled trial. Annals of Medicine and Surgery. 2021; 65:102347. [DOI:10.1016/j.amsu.2021.102347] [PMID] [PMCID]
- Chen YC, Lee CY, Chen SJ. Narcotic addiction in failed back surgery syndrome. Cell Transplantation. 2019; 28(3):239-47. [DOI:10.1177/0963689718796072] [PMID] [PMCID]
- Akshat S, Ramachandran R, Rewari V, Chandralekha, Trikha A, Sinha R. Morphine versus Nalbuphine for open gynaecological surgery: A randomized controlled double blinded trial. Pain Research and Treatment. 2014; 2014:727952. [DOI:10.1155/2014/727952] [PMID] [PMCID]
- Kaushal S, Kamlakar M, Baburao JP. Intrathecal nalbuphine vs. buprenorphine as an adjuvant in lower limb orthopedic surgeries: A prospective randomized controlled study. Medical Gas Research. 2021; 11(4):126-30. [DOI:10.4103/2045-9912.318856] [PMID] [PMCID]
- Malekshoar M, Shafa S, Jahromi MG, Vatankhah M, Adibi P. Pain control in patients undergoing orthopedic surgery: A narrative review study on the role of anesthetics. International Journal of Medical Investigation. 2021; 10(4):41-9. [Link]
- Liu X, Hu J, Hu X, Li R, Li Y, Wong G, et al. Preemptive intravenous nalbuphine for the treatment of post-operative visceral pain: A multicenter, double-blind, placebo-controlled, randomized clinical trial. Pain and Therapy. 2021; 10(2):1155-69. [DOI:10.1007/s40122-021-00275-8] [PMID] [PMCID]
- Zhou L, Yang H, Hai Y, Cheng Y. Perioperative low-dose ketamine for postoperative pain management in spine surgery: A systematic review and meta-analysis of randomized controlled trials. Pain Research & Management. 2022; 2022:1507097.[DOI:10.1155/2022/1507097] [PMID] [PMCID]
- Kaur S, Saroa R, Aggarwal S. Effect of intraoperative infusion of low-dose ketamine on management of postoperative analgesia. Journal of Natural Science, Biology, and Medicine. 2015; 6(2):378-82. [DOI:10.4103/0976-9668.160012] [PMID] [PMCID]
- Wang H, Ma L, Chen Y. Analgesic effects of low-dose ketamine after spinal fusion in adults: A protocol of prospective randomized trial. Medicine. 2020; 99(38):e22162. [DOI:10.1097/MD.0000000000022162] [PMID] [PMCID]
- Etezadi F, Farzizadeh M, Sharifinia HR, Alimohammadi M, Khajavi MR. The effect of intraoperative ketamine and magnesium sulfate on acute pain and opioid consumption after spine surgery. Acta Medica Iranica. 2020; 58(5):221-4. [DOI:10.18502/acta.v58i5.3955]
- Hussein MM, Elhennawy AM. Intravenous lidocaine infusion with single low-dose ketamine as an adjuvant to general anesthesia in posterior spine fusion. Journal of Cellular & Molecular Anesthesia. 2022; 7(2):84-92. [DOI:10.22037/jcma.v7i2.37078]
- Riddell JM, Trummel JM, Onakpoya IJ. Low-dose ketamine in painful orthopaedic surgery: A systematic review and meta-analysis. British Journal of Anaesthesia. 2019; 123(3):325-34. [DOI:10.1016/j.bja.2019.05.043] [PMID]
- Pendi A, Field R, Farhan SD, Eichler M, Bederman SS. Perioperative ketamine for analgesia in spine surgery: A meta-analysis of randomized controlled trials. Spine. 2018; 43(5):E299-307. [DOI:10.1097/BRS.0000000000002318] [PMID] [PMCID]
- Nielsen RV, Fomsgaard JS, Siegel H, Martusevicius R, Nikolajsen L, Dahl JB, et al. Intraoperative ketamine reduces immediate postoperative opioid consumption after spinal fusion surgery in chronic pain patients with opioid dependency: A randomized, blinded trial. Pain. 2017; 158(3):463-70. [DOI:10.1097/j.pain.0000000000000782] [PMID]
- Guay J, Suresh S, Kopp S, Johnson RL. Postoperative epidural analgesia versus systemic analgesia for thoraco-lumbar spine surgery in children. The Cochrane Database of Systematic Reviews. 2019; 1(1):CD012819. [DOI:10.1002/14651858.CD012819.pub2] [PMID] [PMCID]
- Hermans SMM, Lantinga-Zee AAG, Rijkers K, van Santbrink H, van Hemert WLW, Reinders MK, et al. Intraoperative epidural analgesia for pain relief after lumbar decompressive spine surgery: A systematic review and meta-analysis. Brain & Spine. 2021; 1:100306. [DOI:10.1016/j.bas.2021.100306] [PMID] [PMCID]
- Hamed M, Asoglu H, Lampmann T, Winkelmann LM, Salemdawod A, Müller M, et al. Pain management with epidural catheter and epidural analgesia after spinal dorsal instrumentation of lumbar spine. Medicine. 2023; 102(7):e32902. [DOI:10.1097/MD.0000000000032902] [PMID] [PMCID]
- Kumar RJ, Menon KV, Ranjith TC. Use of epidural analgesia for pain management after major spinal surgery. Journal of Orthopaedic Surgery. 2003; 11(1):67-72. [DOI:10.1177/230949900301100114] [PMID]
- Ezhevskaya AA, Mlyavykh SG, Anderson DG. Effects of continuous epidural anesthesia and postoperative epidural analgesia on pain management and stress response in patients undergoing major spinal surgery. Spine. 2013; 38(15):1324-30.[DOI:10.1097/BRS.0b013e318290ff26] [PMID]
- Meng Y, Jiang H, Zhang C, Zhao J, Wang C, Gao R, et al. A comparison of the postoperative analgesic efficacy between epidural and intravenous analgesia in major spine surgery: A meta-analysis. Journal of Pain Research. 2017; 10:405-15.[DOI:10.2147/JPR.S128523] [PMID] [PMCID]
- Waqas M, Shallwani H, Shamim MS, Ahmad K. Perioperative steroids for lumbar disc surgery: A meta-analysis of randomized controlled trials. Surgical Neurology International. 2017; 8:42. [DOI:10.4103/sni.sni_478_16] [PMID] [PMCID]
- Langmayr JJ, Obwegeser AA, Schwarz AB, Laimer I, Ulmer H, Ortler M. Intrathecal steroids to reduce pain after lumbar disc surgery: A double-blind, placebo-controlled prospective study. Pain. 1995; 62(3):357-61. [DOI:10.1016/0304-3959(94)00278-M] [PMID]
- Lotfinia I, Khallaghi E, Meshkini A, Shakeri M, Shima M, Safaeian A. Interaoperative use of epidural methylprednisolone or bupivacaine for postsurgical lumbar discectomy pain relief: A randomized, placebo-controlled trial. Annals of Saudi Medicine. 2007; 27(4):279-83. [DOI:10.5144/0256-4947.2007.279] [PMID] [PMCID]
- Kovarsky D, Shani A, Rod A, Ciubotaru D, Rahamimov N. Effectiveness of intra-venous steroids for preventing surgery for lumbo-sacral radiculopathy secondary to intervertebral disc herniation: A retrospective study of 213 patients. Scientific Reports. 2022; 12(1):6681. [DOI:10.1038/s41598-022-10659-1] [PMID] [PMCID]
- Carassiti M, Pascarella G, Strumia A, Russo F, Papalia GF, Cataldo R, et al. Epidural steroid injections for low back pain: A narrative review. International Journal of Environmental Research and Public Health. 2021; 19(1):231. [DOI:10.3390/ijerph19010231] [PMID] [PMCID]
- Lee JH, Kim DH, Kim DH, Shin KH, Park SJ, Lee GJ, et al. Comparison of clinical efficacy of epidural injection with or without steroid in lumbosacral disc herniation: A systematic review and meta-analysis. Pain Physician. 2018; 21(5):449-68. [DOI:10.36076/ppj.2018.5.449] [PMID]
- Samoladas E, Kapinas A, Papadopoulos DV, Gkiatas I, Papastefanou S, Gelalis ID. Intraoperative epidural application of steroid and local anaesthetic agent following lumbar discectomy: A prospective double blinded randomized controlled trial. Journal of Clinical Orthopaedics and Trauma. 2019; 10(Suppl 1):S143-6. [DOI:10.1016/j.jcot.2019.03.005] [PMID] [PMCID]
- Lee SM, Yun DJ, Lee SH, Lee HC, Joeng KH. Continuous wound infiltration of ropivacaine for reducing of postoperative pain after anterior lumbar fusion surgery: A clinical retrospective comparative study. The Korean Journal of Pain. 2021; 34(2):193-200. [DOI:10.3344/kjp.2021.34.2.193] [PMID] [PMCID]
- Stamenkovic DM, Bezmarevic M, Bojic S, Unic-Stojanovic D, Stojkovic D, Slavkovic DZ, et al. Updates on wound infiltration use for postoperative pain management: A narrative review.Journal of Clinical Medicine. 2021; 10(20):4659. [DOI:10.3390/jcm10204659] [PMID] [PMCID]
- Kjærgaard M, Møiniche S, Olsen KS. Wound infiltration with local anesthetics for post-operative pain relief in lumbar spine surgery: A systematic review. Acta Anaesthesiologica Scandinavica. 2012; 56(3):282-90. [DOI:10.1111/j.1399-6576.2011.02629.x] [PMID]
- Li K, Ji C, Luo D, Feng H, Yang K, Xu H. Wound infiltration with ropivacaine as an adjuvant to patient controlled analgesia for transforaminal lumbar interbody fusion: A retrospective study. BMC Anesthesiology. 2020; 20(1):288. [DOI:10.1186/s12871-020-01205-5] [PMID] [PMCID]
- Scott NB. Wound infiltration for surgery. Anaesthesia. 2010; 65(Suppl 1):67-75. [DOI:10.1111/j.1365-2044.2010.06241.x] [PMID]
- Jirarattanaphochai K, Jung S. Nonsteroidal antiinflammatory drugs for postoperative pain management after lumbar spine surgery: A meta-analysis of randomized controlled trials. Journal of Neurosurgery. Spine. 2008; 9(1):22-31. [DOI:10.3171/SPI/2008/9/7/022] [PMID]
- Zhang Z, Xu H, Zhang Y, Li W, Yang Y, Han T, et al. Nonsteroidal anti-inflammatory drugs for postoperative pain control after lumbar spine surgery: A meta-analysis of randomized controlled trials. Journal of Clinical Anesthesia. 2017; 43:84-9. [DOI:10.1016/j.jclinane.2017.08.030] [PMID]
- Khoo B, Crene E, Le D, Ng W. Perioperative NSAID use in single level microdiscectomy and hemilaminectomy. Interdisciplinary Neurosurgery. 2023; 31:101679. [DOI:10.1016/j.inat.2022.101679]
- Ma N, Yi P, Xiong Z, Ma H, Tan M, Tang X. Efficacy and safety of perioperative use of non-steroidal anti-inflammatory drugs for preemptive analgesia in lumbar spine surgery: A systematic review and meta-analysis. Perioperative Medicine. 2023; 12(1):61. [DOI:10.1186/s13741-023-00347-7] [PMID][PMCID]
- Friedman BW, Dym AA, Davitt M, Holden L, Solorzano C, Esses D, et al. Naproxen with cyclobenzaprine, oxycodone/acetaminophen, or placebo for treating acute low back pain: A randomized clinical trial. JAMA. 2015; 314(15):1572-80. [DOI:10.1001/jama.2015.13043] [PMID]
- Onda A, Ogoshi A, Itoh M, Nakagawa T, Kimura M. Comparison of the effects of treatment with celecoxib, loxoprofen, and acetaminophen on postoperative acute pain after arthroscopic knee surgery: A randomized, parallel-group trial. Journal of Orthopaedic Science. 2016; 21(2):172-7. [DOI:10.1016/j.jos.2015.11.005] [PMID]
- Kumar SS, Kumar A, Talawar P, Kaushal A, Rekha, Sangadala P, et al. Peripheral nerve blocks for the management of lumbo-sacral radiculopathy: A prospective study. Saudi Journal of Anaesthesia. 2023; 17(3):353-8. [DOI:10.4103/sja.sja_880_22] [PMID] [PMCID]
- Jogie J, Jogie JA. A comprehensive review on the efficacy of nerve blocks in reducing postoperative anesthetic and analgesic requirements. Cureus. 2023; 15(5):e38552. [DOI:10.7759/cureus.38552]
- Joshi G, Gandhi K, Shah N, Gadsden J, Corman SL. Peripheral nerve blocks in the management of postoperative pain: Challenges and opportunities. Journal of Clinical Anesthesia. 2016; 35:524-9. [DOI:10.1016/j.jclinane.2016.08.041] [PMID]
- Adabala V, Talawar P, Kumar A, Mohanta J, Suresh S. Effect of peripheral nerve blocks with low dose lignocaine for the treatment of acute lumbosacral radiculopathy: A pilot study. Archives of Anesthesiology and Critical Care. 2020; 6(3):109-11. [DOI:10.18502/aacc.v6i3.3993]
- Tsai SHL, Hu CW, El Sammak S, Durrani S, Ghaith AK, Lin CCJ, et al. Different gabapentin and pregabalin dosages for perioperative pain control in patients undergoing spine surgery: A systematic review and network meta-analysis. JAMA Network Open. 2023; 6(8):e2328121. [DOI:10.1001/jamanetworkopen.2023.28121] [PMID] [PMCID]
- Routray SS, Pani N, Mishra D, Nayak S. Comparison of pregabalin with gabapentin as preemptive analgesic in lumbar spine surgery. Journal of Anaesthesiology, Clinical Pharmacology. 2018; 34(2):232-6. [DOI:10.4103/joacp.JOACP_12_17] [PMID] [PMCID]
- Yu L, Ran B, Li M, Shi Z. Gabapentin and pregabalin in the management of postoperative pain after lumbar spinal surgery: A systematic review and meta-analysis. Spine. 2013; 38(22):1947-52. [DOI:10.1097/BRS.0b013e3182a69b90] [PMID]
- Terai H, Tamai K, Kaneda K, Omine T, Katsuda H, Shimada N, et al. Postoperative physical therapy program focused on low back pain can improve treatment satisfaction after minimally invasive lumbar decompression. Journal of Clinical Medicine. 2022; 11(19):5566. [DOI:10.3390/jcm11195566] [PMID] [PMCID]
- Manni T, Ferri N, Vanti C, Ferrari S, Cuoghi I, Gaeta C, et al. Rehabilitation after lumbar spine surgery in adults: A systematic review with meta-analysis. Archives of Physiotherapy. 2023; 13(1):21. [DOI:10.1186/s40945-023-00175-4] [PMID] [PMCID]
- Afzal K, Khattak HG, Sajjad AG, Hussain SA, Sarfraz Z, Sarfraz A, et al. Impact of active physiotherapy rehabilitation on pain and global and functional improvement 1-2 months after lumbar disk surgery: A systematic review and meta-analysis. Healthcare. 2022; 10(10):1943. [DOI:10.3390/healthcare10101943] [PMID] [PMCID]
- Ozkara GO, Özgen M, Ozkara E, Armagan O, Arslantaş A, Atasoy MA. Effectiveness of physical therapy and rehabilitation programs starting immediately after lumbar disc surgery. Turkish Neurosurgery. 2015; 25(3):372-9. [Link]
- Zhu Y, Xia S, Yang W, Shi F, Ji H. Early efficacy of postoperative rehabilitation training for lumbar disc herniation. BMc Sports Science, Medicine & Rehabilitation. 2023; 15(1):97. [DOI:10.1186/s13102-023-00704-5] [PMID] [PMCID]
- Atsidakou N, Matsi AE, Christakou A. The effectiveness of exercise program after lumbar discectomy surgery. Journal of Clinical Orthopaedics and Trauma. 2021; 16:99-105. [DOI:10.1016/j.jcot.2020.12.030] [PMID] [PMCID]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



